Scleroderma is a rare autoimmune disease that affects the body’s connective tissue. It causes the skin and organs to harden and tighten. When someone has scleroderma, their body produces too much collagen, leading to thickening and scarring of various tissues.
The effects of scleroderma can vary from person to person. Some may only experience skin changes, while others might have problems with internal organs. The disease can impact blood vessels, muscles, and joints.
Scleroderma can cause many changes in the body. It may lead to dry, itchy skin, joint pain, and difficulty swallowing. In some cases, it can affect the heart, lungs, and kidneys. Early detection and treatment are key to managing symptoms and slowing disease progression.
Key Takeaways
- Scleroderma causes the body to produce excess collagen, leading to hardening of skin and organs.
- The disease can affect various parts of the body, from skin to internal organs.
- Early diagnosis and proper management are crucial for controlling scleroderma symptoms.
Understanding Scleroderma
Scleroderma is a complex autoimmune disease that affects the body’s connective tissues. It causes hardening and tightening of the skin and can impact internal organs.
Defining Scleroderma
Scleroderma is a rare condition that results from the overproduction of collagen in the body. This excess collagen builds up in the skin and organs, leading to various symptoms.
The name “scleroderma” comes from the Greek words “sclero” meaning hard, and “derma” meaning skin. This describes the main feature of the disease – hardening of the skin.
Scleroderma affects each person differently. Some may have mild symptoms, while others experience severe complications.
Different Types of Scleroderma
There are two main types of scleroderma: localized and systemic.
Localized scleroderma mainly affects the skin. It doesn’t spread to internal organs and is generally less serious.
Systemic scleroderma, also called systemic sclerosis, affects both the skin and internal organs. It can be further divided into limited and diffuse forms.
Limited systemic sclerosis typically affects the skin on the face, hands, and feet. It may also impact the digestive system and lungs.
Diffuse systemic sclerosis can affect larger areas of skin and multiple internal organs.
Scleroderma vs. Systemic Sclerosis
The terms scleroderma and systemic sclerosis are often used interchangeably, but they’re not exactly the same.
Scleroderma is a broader term that includes all forms of the disease, both localized and systemic.
Systemic sclerosis specifically refers to the systemic form of scleroderma. It always involves internal organs along with skin changes.
CREST syndrome is a limited form of systemic sclerosis. CREST stands for:
- Calcinosis (calcium deposits in the skin)
- Raynaud’s phenomenon
- Esophageal dysfunction
- Sclerodactyly (skin tightening on fingers)
- Telangiectasias (dilated blood vessels)
Prevalence and Epidemiology
Scleroderma is considered a rare disease. It affects about 300 per 1 million people in the United States.
Women are more likely to develop scleroderma than men. The disease typically starts between ages 30 and 50.
Scleroderma can occur in children, but this is less common. When it does, it’s usually the localized form.
Certain factors may increase the risk of developing scleroderma:
- Genetics
- Environmental triggers
- Occupational exposure to certain chemicals
African Americans and some Native Americans have higher rates of the disease and may experience more severe symptoms.
Symptoms and Early Detection
Scleroderma affects people differently. Symptoms can range from mild to severe. Early detection is key for better management of the disease.
Early Symptoms
Raynaud’s phenomenon is often one of the first signs of scleroderma. It causes fingers and toes to feel cold and numb when exposed to cold or stress. The skin may change color, turning white, blue, or red.
Skin changes are another early symptom. The skin may become puffy or swollen, especially on the hands and fingers. It might feel tight or itchy.
Some people notice joint pain and stiffness. This can make it hard to move fingers or other joints freely.
Progression of Symptoms
As scleroderma progresses, symptoms can worsen. Skin tightening may spread to other parts of the body. This can limit movement and cause discomfort.
Digestive issues may develop. These can include:
- Heartburn
- Difficulty swallowing
- Bloating
- Constipation or diarrhea
Fatigue is common. People may feel tired even after a full night’s sleep.
Shortness of breath might occur if the lungs are affected. This can make physical activities harder.
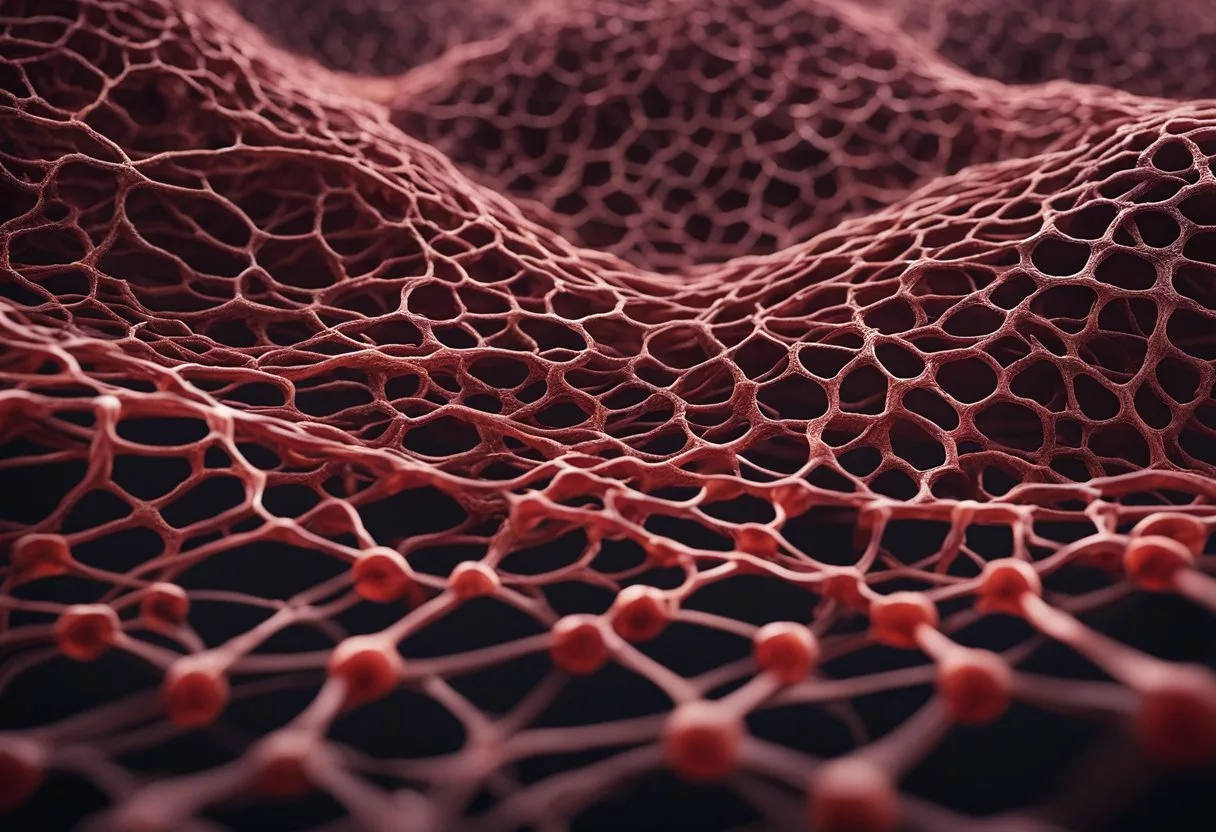
Skin-Related Manifestations
Skin thickening is a hallmark of scleroderma. It often starts in the fingers and hands. The skin can become hard and shiny.
Telangiectasia are small red spots on the skin. They’re caused by widened blood vessels. These spots are common on the face, hands, and lips.
Calcinosis is another skin issue. It causes small, hard lumps to form under the skin. These lumps contain calcium deposits.
Some people develop skin ulcers. These are open sores that can be painful and slow to heal.
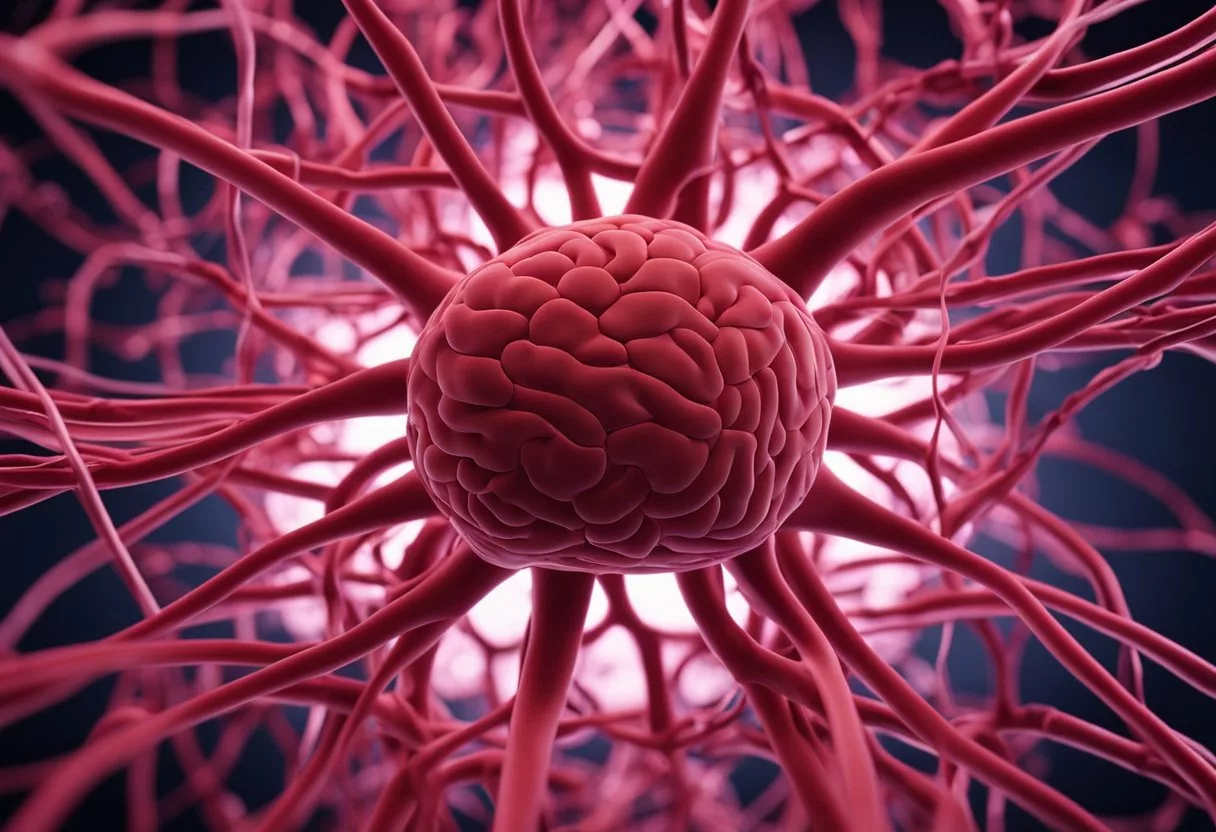
Internal Organ Involvement
Scleroderma can affect internal organs. This is called systemic sclerosis. It’s important to watch for signs of organ involvement.
Lung problems can cause shortness of breath and a dry cough. These symptoms may worsen over time.
Heart issues might include chest pain or an irregular heartbeat. These need prompt medical attention.
Kidney problems can lead to high blood pressure. In severe cases, it can cause kidney failure.
Some people have sclerosis sine scleroderma. This type affects internal organs without causing major skin changes.
Systemic Impact of Scleroderma
Scleroderma affects multiple organs and systems in the body. It causes changes in blood vessels, tissues, and organs. These changes can lead to serious health issues.
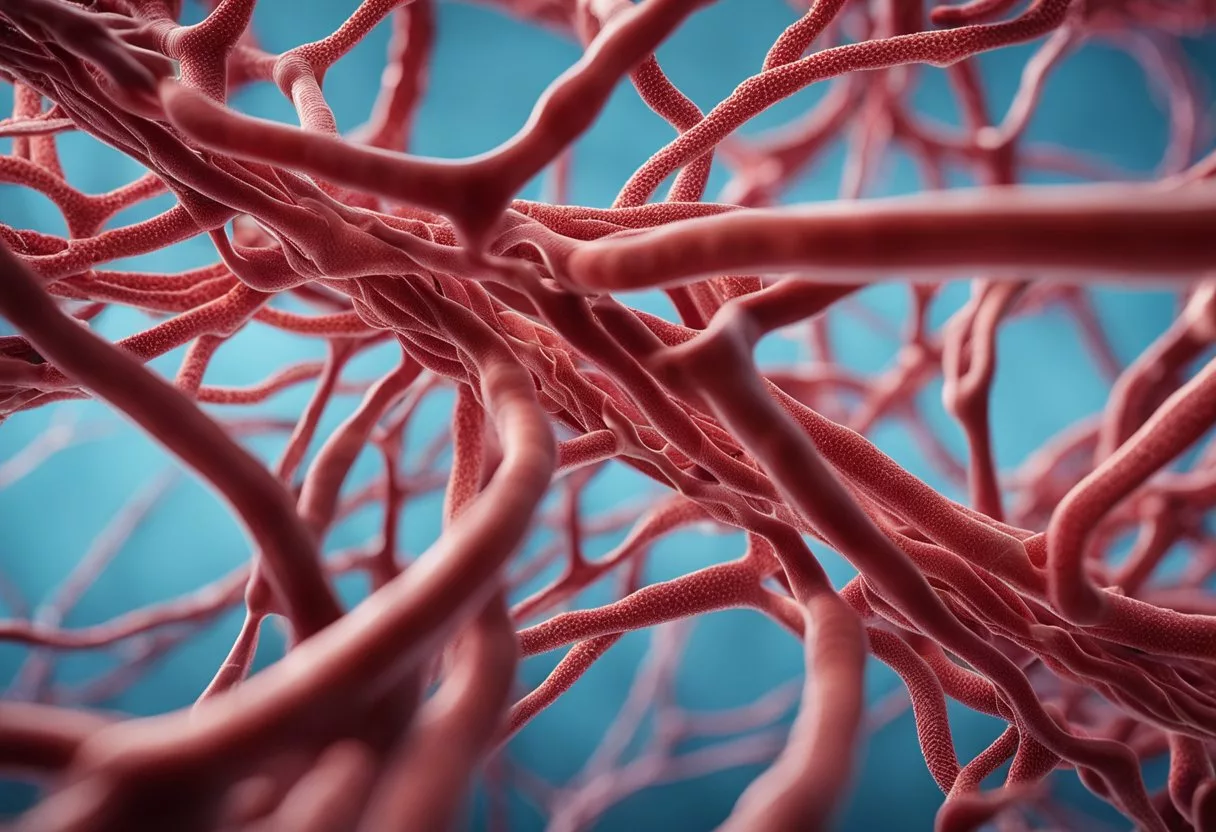
Vascular System Effects
Scleroderma impacts small blood vessels throughout the body. It causes them to narrow and harden. This reduces blood flow to affected areas.
People may notice:
- Cold fingers and toes
- Skin color changes
- Sores on fingertips
These symptoms can be painful and make daily tasks hard. In severe cases, reduced blood flow may lead to tissue damage.
Pulmonary Complications
Scleroderma can cause serious lung problems. It may lead to:
- Pulmonary fibrosis (scarring of lung tissue)
- Pulmonary hypertension (high blood pressure in lung arteries)
These issues make breathing harder. People might feel short of breath, especially when active. Lung damage can worsen over time if not treated.
Gastrointestinal Tract Issues
The digestive system is often affected by scleroderma. Common problems include:
- Acid reflux
- Trouble swallowing
- Slow digestion
- Bloating and constipation
These symptoms can make eating uncomfortable. They may lead to weight loss and malnutrition if not managed well.
Renal and Cardiac Involvement
Scleroderma can harm the kidneys and heart. Key issues include:
- Kidney problems:
- Scleroderma renal crisis (sudden high blood pressure and kidney failure)
- Protein in urine
- Heart complications:
- Irregular heartbeat
- Heart muscle scarring
- Fluid around the heart
These problems can be life-threatening if not caught early. Regular check-ups are crucial for people with scleroderma.
Musculoskeletal Symptoms
Scleroderma affects muscles, joints, and connective tissues. People may experience:
- Joint pain and stiffness
- Muscle weakness
- Tendon friction rubs
These symptoms can limit movement and daily activities. Exercise and physical therapy can help maintain flexibility and strength.
Diagnostic Processes
Doctors use several methods to diagnose scleroderma. These include physical exams, blood tests, and imaging studies. Each step helps identify key signs of the disease.
Initial Clinical Assessment
A doctor starts by looking at the patient’s skin. They check for hard or thickened areas, especially on the hands and face. The doctor also looks for swelling in the fingers and toes.
They ask about symptoms like Raynaud’s phenomenon. This is when fingers turn white or blue in cold weather. The doctor checks for tiny red spots called telangiectasias on the skin.
The patient’s medical history is important. The doctor asks about exposure to chemicals, silica, or solvents. These may trigger scleroderma in some people.
Laboratory Tests
Blood tests play a key role in diagnosis. They look for signs of autoimmune activity. Common tests include:
- Antinuclear antibody (ANA) test
- Scl-70 antibody test
- Anticentromere antibody test
These tests help show if the immune system is attacking healthy tissue. They also help rule out other autoimmune disorders.
Doctors may check for inflammation markers. High levels can point to active disease. Genetic tests might be done to look for inherited risk factors.
Imaging and Other Diagnostic Tools
Imaging tests help doctors see internal changes caused by scleroderma. X-rays can show lung damage. CT scans give a more detailed view of organs.
Echocardiograms check heart function. They can spot problems with heart valves or blood pressure in the lungs.
Skin biopsies may be taken. These small samples of skin are examined under a microscope. They can show thickening of collagen fibers.
Pulmonary function tests measure how well the lungs work. This is important because scleroderma can affect breathing.
Potential Causes and Risk Factors
The exact cause of scleroderma is unknown. Scientists think it may result from a mix of genetic and environmental factors. These factors can affect how the immune system works.
Genetic Predisposition
Some people may be born with genes that make them more likely to get scleroderma. Certain genes can increase the risk of developing the condition. But having these genes doesn’t mean a person will definitely get scleroderma.
Family history can play a role. If someone in a family has scleroderma, other family members have a slightly higher chance of getting it too.
Still, most people with scleroderma don’t have any family members with the disease. This suggests that genes alone don’t cause scleroderma.
Environmental Factors
The environment may trigger scleroderma in people who are already at risk. Some environmental factors that might increase the risk include:
- Exposure to silica dust
- Contact with certain chemicals or solvents
- Viral infections
Men who work with silica seem to have a higher risk of getting scleroderma. Some drugs may also raise the risk.
Injuries or stress to the skin or joints might play a role in some cases. But more research is needed to understand how these factors affect scleroderma risk.
Immune System Function
In scleroderma, the immune system attacks the body’s own tissues. This leads to inflammation and scarring. The immune system usually protects the body from harm. But in scleroderma, it doesn’t work right.
Autoimmune diseases like lupus (about 20% of lupus patients will develop scleroderma) or rheumatoid arthritis may be associated with scleroderma. These conditions also involve problems with the immune system.
Women (80% of cases) are more likely than men to get scleroderma. The disease often starts between ages 30 and 50. These facts suggest that hormones might play a role in how the immune system works in scleroderma.
Management and Treatment

Scleroderma treatment aims to control symptoms and prevent organ damage. Doctors use various approaches to manage this complex condition.
General Treatment Approaches
Scleroderma treatment focuses on addressing specific symptoms and organ involvement. There’s no one-size-fits-all approach. Doctors create personalized plans based on each patient’s needs.
Treatment goals include:
- Reducing inflammation
- Controlling blood pressure
- Easing pain and discomfort
- Slowing disease progression
- Improving quality of life
Regular check-ups are crucial. They help catch and treat complications early.
Medications and Drugs
Doctors may prescribe several types of medications to manage scleroderma:
- Immunosuppressants: These drugs calm the overactive immune system.
- Blood pressure medications: They help control high blood pressure, a common scleroderma complication.
- Pain relievers: Over-the-counter or prescription options can ease discomfort.
- Acid reflux medications: These help manage digestive symptoms.
Some patients might need drugs to treat specific organ problems. For example, lung or kidney issues may require targeted medications.
Physical Therapy and Lifestyle Modifications
Physical therapy plays a key role in scleroderma management. It helps maintain joint flexibility and muscle strength.
Lifestyle changes can also make a big difference:
- Regular exercise: Keeps joints flexible and improves circulation
- Skin care: Moisturizing helps manage skin tightness
- Diet changes: Some foods may worsen symptoms
- Stress management: Stress can trigger flare-ups
Occupational therapy can help patients adapt daily activities to their changing abilities.
Experimental Therapies
Research into new scleroderma treatments is ongoing. Some experimental therapies show promise:
- Stem cell transplants: May reset the immune system
- New biologics: Target specific parts of the immune response
- Gene therapy: Aims to correct genetic factors linked to scleroderma
Clinical trials offer access to these cutting-edge treatments. However, they may carry risks. Patients should discuss options with their doctors.
Remember, while there’s no cure for scleroderma yet, proper management can greatly improve quality of life.
Living With Scleroderma
Scleroderma affects daily life in many ways. People with this condition face challenges but can find ways to cope and thrive.
Quality of Life Factors
Scleroderma can impact a person’s quality of life. Fatigue is common and may limit activities. Skin tightening can make movement difficult.
Pain and stiffness in joints can affect work and hobbies. Breathing problems may restrict physical activity. Digestive issues can change eating habits.
Despite these challenges, many people with scleroderma lead full lives. They adapt their routines and find new ways to do things they enjoy. Proper treatment helps manage symptoms and improve comfort.
Emotional and Psychological Support
Living with scleroderma can be emotionally tough. Feelings of anxiety or depression are normal. Getting support is key.
Talking to a therapist can help process emotions. Support groups connect people with similar experiences. Sharing concerns and tips can be comforting.
Family and friends play a vital role too. Their understanding and help make a big difference. Learning stress management techniques like meditation can also boost mental well-being.
Patient Education and Resources
Knowledge is power when dealing with scleroderma. Learning about the condition helps people make informed decisions.
The Scleroderma Research Foundation offers up-to-date information. Local scleroderma centers often provide educational programs. These teach about symptoms, treatments, and coping strategies.
Online forums let patients share advice and experiences. Some hospitals have special clinics for scleroderma care. These offer expert treatment and the latest research findings.
Patients should ask their doctors about new studies or clinical trials. Staying informed about advances in scleroderma research gives hope for better treatments.
Outlook and Future Directions
Scleroderma research is making progress. New treatments offer hope for better outcomes. Scientists are working hard to find a cure.
Research and Developments
Scientists are learning more about scleroderma every day. They’re studying how the immune system affects the disease. This helps them find new ways to treat it.
Researchers are looking at genes linked to scleroderma. This may help predict who might get it. It could also lead to new treatments.
Studies are testing new drugs to slow the disease. Some target specific parts of the immune system. Others aim to stop scarring in the skin and organs.
Advancements in Treatments
New treatments for scleroderma are being tested. Some focus on easing symptoms. Others try to stop the disease from getting worse.
Stem cell therapy shows promise. It may help reset the immune system. This could slow or stop the disease.
Doctors are trying new ways to use existing drugs. They’re combining treatments to get better results. This may help patients feel better and live longer.
Prospects for a Cure
A cure for scleroderma is not yet found. But scientists are hopeful. They’re working hard to understand the disease better.
New tools let researchers study scleroderma at the cell level. This may lead to breakthroughs in treatment.
Clinical trials are testing new ideas. Some look at ways to reverse skin hardening. Others try to heal damaged organs.
While a cure is the goal, current research aims to improve life for patients. Better treatments can help people with scleroderma live longer, healthier lives.
Frequently Asked Questions
Scleroderma is a complex condition that affects people differently. It can cause various symptoms and complications, and its progression and triggers are not fully understood.
What are the common symptoms experienced in the early stages of scleroderma?
Early signs of scleroderma often include skin changes. People may notice tightening and thickening of the skin, especially on the hands and face.
Raynaud’s phenomenon is another common early symptom. This causes fingers and toes to become cold and numb in response to stress or cold temperatures.
How does scleroderma typically progress over time?
Scleroderma progression varies from person to person. Some may experience mild symptoms that develop slowly over years.
Others may have rapid progression with more severe effects. The disease can spread to affect larger areas of skin and internal organs over time.
Can scleroderma affect internal organs, and what are the signs?
Yes, scleroderma can affect internal organs. Signs of organ involvement may include:
- Shortness of breath (lungs)
- Difficulty swallowing (esophagus)
- Heartburn or acid reflux (digestive system)
- High blood pressure (kidneys)
Is there a genetic component to scleroderma, and can it run in families?
While scleroderma is not directly inherited, there may be a genetic predisposition. People with certain genes might be more likely to develop the condition.
Having a family member with scleroderma slightly increases the risk, but most cases occur in people with no family history.
What are the potential complications associated with advanced scleroderma?
Advanced scleroderma can lead to serious complications. These may include:
- Pulmonary hypertension
- Kidney failure
- Heart problems
- Malnutrition due to digestive issues
The severity and type of complications depend on which organs are affected.
Are there any known triggers or underlying causes of scleroderma?
The exact cause of scleroderma is unknown. It’s believed to be an autoimmune disease where the immune system attacks healthy tissue.
Some potential triggers may include:
- Exposure to certain chemicals or toxins
- Viral infections
- Hormonal changes
More research is needed to fully understand what triggers scleroderma.