Let’s try to clarify this concept first. There is no such thing of “TNBC of the skin”. When people look for information, they are looking for the cutaneous or skin manifestations of triple-negative breast cancer (TNBC).
Triple-negative breast cancer is a subtype of breast cancer that lacks the expression of estrogen receptors (ER), progesterone receptors (PR), and human epidermal growth factor receptor 2 (HER2). This type of cancer is more aggressive and has a poorer prognosis than other types of breast cancer. TNBC can metastasize to other organs, including the skin, leading to specific cutaneous symptoms that require distinct treatments. Skin metastasis is a rare manifestation of TNBC, but it can occur in up to 24% of patients with advanced TNBC [1].
TNBC is a heterogeneous disease, and the molecular mechanisms underlying the development and progression of TNBC skin metastasis are not fully understood. However, recent studies have identified several factors that may contribute to the development of skin metastasis in TNBC, including tumor heterogeneity, genetic mutations, and the interaction between tumor cells and the microenvironment [2]. Understanding the pathophysiology of TNBC skin metastasis is critical for the development of effective treatments and improving patient outcomes. In this article, we will explore the clinical presentation, diagnostic procedures, treatment strategies, and prognosis of TNBC skin metastasis.
Get TNBC Bracelets Here[3]
Key Takeaways
-
- TNBC is a subtype of breast cancer that lacks the expression of ER, PR, and HER2 and has a poorer prognosis than other types of breast cancer.
-
- Skin metastasis is a rare manifestation of TNBC, but it can occur in up to 24% of patients with advanced TNBC.
-
- Understanding the pathophysiology of TNBC skin metastasis is critical for the development of effective treatments and improving patient outcomes.
Understanding TNBC
Definition of Triple-Negative Breast Cancer (TNBC)
Triple-negative breast cancer (TNBC) is a subtype of breast cancer that lacks the expression of estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2). According to Cancer.org[4], TNBC accounts for about 10-15% of all breast cancers. TNBC is known for its aggressive nature, fast growth, and high chances of recurrence.
Biological Characteristics of TNBC
TNBC is a challenging subtype distinguished by what it lacks compared to other forms of breast cancer. TNBC cells do not express the receptors that are targeted by current hormone therapies, making it difficult to treat. TNBC is more common in younger women, African American women, and women with BRCA1 gene mutations.
TNBC is classified as a basal-like subtype of breast cancer, which means that the cancer cells have similar characteristics to basal cells found in the breast ducts. Basal-like cancers are more likely to be triple-negative and grow rapidly.
In summary, TNBC is a subtype of breast cancer that lacks the expression of ER, PR, and HER2 receptors. TNBC is more aggressive and has a higher chance of recurrence than other forms of breast cancer. TNBC is classified as a basal-like subtype of breast cancer and is more common in younger women, African American women, and women with BRCA1 gene mutations.
Epidemiology and Risk Factors
Triple-Negative Breast Cancer (TNBC) is a type of breast cancer defined by the absence of estrogen and progesterone hormone receptors and the HER2 protein. TNBC is a rare subtype of breast cancer, accounting for only 10-20% of all breast cancers. However, TNBC is more aggressive and has a poorer prognosis than other types of breast cancer.
Prevalence in Different Populations
TNBC is more common in certain populations, including younger women, African American women, and women with BRCA1 mutations. TNBC is more common in women under the age of 50, with approximately 20% of breast cancer cases occurring in women under the age of 45. African American women are more likely to develop TNBC than women of other races. In fact, African American women are three times more likely to develop TNBC than white women.
Identifying Risk Factors
Identifying risk factors for TNBC is important for early detection and prevention. Some of the known risk factors for TNBC include obesity, lack of physical activity, and a family history of breast cancer. Women with a BRCA1 mutation are also at increased risk of developing TNBC. However, most women with TNBC do not have a family history of breast cancer or a known genetic mutation.
While there is no sure way to prevent TNBC, there are steps that women can take to reduce their risk. Maintaining a healthy weight, exercising regularly, and limiting alcohol consumption are all important steps in reducing the risk of breast cancer. Women should also be aware of any changes in their breasts and report any unusual symptoms to their healthcare provider.
In conclusion, TNBC is a rare but aggressive subtype of breast cancer. African American women and women with BRCA1 mutations are at increased risk of developing TNBC. Identifying risk factors and taking steps to reduce the risk of breast cancer is important for early detection and prevention.
Clinical Presentation

Triple-negative breast cancer (TNBC) is a rare form of invasive breast cancer that lacks receptors for estrogen, progesterone, and HER-2/neu genes. TNBC can also present on the skin, and it is important to recognize cutaneous symptoms that may indicate the presence of TNBC.
Common Symptoms of TNBC
TNBC skin manifestations may present as rapidly growing nodules or as an inflammatory process that resembles a skin infection. According to a study[5] published in the Journal of Breast Cancer, skin metastasis can present clinically in various patterns. For example, it can present as new skin nodules, the most common presentation, or ulcers, which are relatively less common. Other rarer clinical manifestations include erythematous patches or plaques.
Physical Signs and Examination
Precise staging helps guide clinical decisions, impacting prognosis. Staging of Breast Cancer is crucial to determine the extent of the disease and the best course of treatment. The physical examination of the breast and axilla is important to identify any palpable masses, skin dimpling, nipple retraction, or nipple discharge. According to the Cleveland Clinic[6], TNBC may present with a lump or swelling in the breast, but it is usually painless. However, breast pain may be present in some cases.
Overall, recognizing the clinical presentation of TNBC is important to provide early diagnosis and treatment. If a patient presents with any of the symptoms or physical signs associated with TNBC, prompt referral to a specialist is recommended.
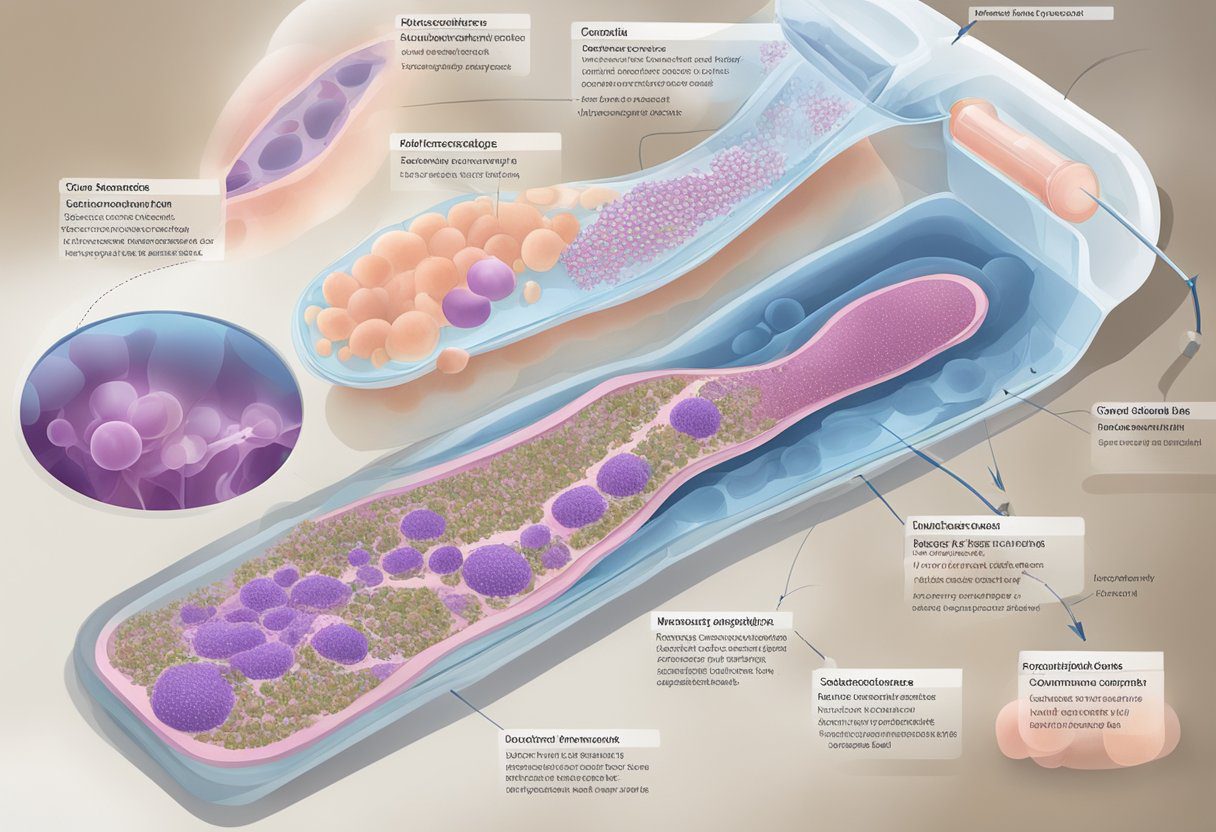
Diagnostic Procedures

Imaging and Biopsy Techniques
The diagnosis of TNBC of the skin is made through a combination of physical examination, imaging tests, and biopsy. Imaging tests such as mammogram, ultrasound, and magnetic resonance imaging (MRI) may be used to evaluate the extent of the disease and to determine if it has spread to nearby lymph nodes or other parts of the body. Imaging tests can also help guide the biopsy procedure.
Biopsy is the most important diagnostic test for TNBC of the skin. A biopsy involves removing a small sample of tissue from the affected area and examining it under a microscope to look for cancer cells. There are several types of biopsy techniques, including punch biopsy, incisional biopsy, and excisional biopsy. The choice of biopsy technique depends on the size and location of the lesion.
Staging and Grading of TNBC
After the diagnosis of TNBC of the skin is confirmed, staging and grading are performed to determine the extent and aggressiveness of the disease. Staging is the process of determining the size of the tumor and whether it has spread to nearby lymph nodes or other parts of the body. Staging is important because it helps guide treatment decisions and provides information about prognosis.
Grading is the process of evaluating the appearance of cancer cells under a microscope to determine how abnormal they look compared to normal cells. The grade of TNBC of the skin is important because it provides information about how fast the cancer is growing and how likely it is to spread. TNBC of the skin is usually graded using the Nottingham Histologic Grade (NHG) system, which assigns a score based on the degree of differentiation, tubule formation, and mitotic activity of the cancer cells.
In addition to imaging tests, biopsy, staging, and grading, clinical trials may be available for patients with TNBC of the skin. Clinical trials are research studies that evaluate new treatments or procedures for cancer. They may offer patients access to new treatments that are not yet available to the general public.
Treatment Strategies
Treatment strategies for TNBC of the skin depend on the stage of cancer, the patient’s overall health, and the extent of skin involvement. A multidisciplinary team of healthcare professionals, including medical oncologists, radiation oncologists, and dermatologists, work together to develop a personalized treatment plan for each patient.
Surgical Interventions
Surgical interventions are the primary treatment option for TNBC of the skin. Lumpectomy, mastectomy, and breast-conserving surgery are the most common surgical interventions. In some cases, the surgical removal of the skin lesion may be necessary. The goal of surgery is to remove all cancerous tissue and prevent the spread of cancer to other parts of the body. The type of surgery depends on the size and location of the tumor.
Chemotherapy and Radiation
Chemotherapy and radiation therapy are common treatment options for TNBC of the skin. Platinum chemotherapy is an effective treatment option for TNBC. Cisplatin is a platinum-based chemotherapy drug that is used to treat TNBC of the skin. Radiation therapy is also an effective treatment option for TNBC of the skin. Radiation therapy uses high-energy x-rays to destroy cancer cells. It is often used in combination with chemotherapy to increase the effectiveness of treatment.
Emerging Therapies
Emerging therapies are being developed to treat TNBC of the skin. Antibody-drug conjugates and targeted therapies are promising treatment options for TNBC. Antibody-drug conjugates are a type of targeted therapy that delivers chemotherapy directly to cancer cells. Targeted therapies are drugs that target specific proteins or genes that are involved in cancer growth. Neoadjuvant chemotherapy is another emerging therapy that is being used to treat TNBC. It is a type of chemotherapy that is given before surgery to shrink the size of the tumor.
In conclusion, TNBC of the skin requires a personalized treatment plan that takes into account the patient’s overall health and the extent of skin involvement. Surgical interventions, chemotherapy and radiation, and emerging therapies are all effective treatment options. A multidisciplinary team of healthcare professionals works together to develop the most effective treatment plan for each patient.
Get TNBC Apparel Here[7]
Prognosis and Survival
Triple-Negative Breast Cancer (TNBC) is a rare and aggressive form of breast cancer that lacks the three most common receptors found in breast cancer cells: estrogen, progesterone, and HER2. When TNBC spreads to the skin, it can cause cutaneous symptoms such as new lumps, skin metastasis, and skin breakdown [1]. The prognosis of TNBC varies, with survival rates and recurrence being key factors affecting patient outcomes.
Factors Influencing Prognosis
Several factors can influence the prognosis of TNBC of the skin, including the stage of the cancer, the size of the tumor, the presence of lymph node involvement, and the grade of the tumor. TNBC that has spread to the skin is usually classified as stage IV cancer, which means that it has metastasized to other parts of the body [2].
Survival Rates and Recurrence
The five-year survival rate for TNBC is approximately 77%, contrasting with a 91% survival rate for all breast cancers combined [1]. However, the survival rate for patients with TNBC that has spread to the skin is lower than that of patients with TNBC that has not spread to the skin. Patients with metastatic TNBC have a poor prognosis, with a median overall survival of 13.3 months [4].
The recurrence rate of TNBC is also higher than that of other breast cancers. TNBC is more likely to recur within the first three years after treatment, and the risk of recurrence remains high for up to five years after treatment [1].
In conclusion, TNBC of the skin is a rare and aggressive form of breast cancer that can cause cutaneous symptoms such as skin metastasis and skin breakdown. The prognosis of TNBC varies depending on several factors, including the stage of the cancer, the size of the tumor, the presence of lymph node involvement, and the grade of the tumor. Patients with TNBC that has spread to the skin have a lower survival rate than those with TNBC that has not spread to the skin, and the recurrence rate of TNBC is also higher than that of other breast cancers.
References:
Support and Management

After a diagnosis of TNBC of the skin, it is important to have support and a management plan in place. Coping with side effects, follow-up care, and long-term care are all essential components of managing TNBC of the skin.
Coping with Side Effects
TNBC of the skin treatment can cause side effects that vary depending on the type of treatment used. Patients may experience fatigue, skin irritation, and hair loss. Healthcare professionals can help manage these side effects by offering suggestions for managing symptoms and prescribing medication to alleviate discomfort.
Patients can also seek support from a variety of sources, including support groups and counseling. Support groups can provide a community of people who understand the challenges of living with TNBC of the skin and offer comfort and guidance. Counseling can help patients cope with the emotional impact of the diagnosis and treatment.
Follow-up and Long-term Care
After treatment for TNBC of the skin, patients will need to follow up with their healthcare professional to monitor their progress and manage any long-term side effects. Follow-up care may include regular checkups, imaging tests, and blood tests. Patients should also be aware of any potential signs of recurrence and report them to their healthcare professional immediately.
Long-term care may involve ongoing treatment to manage side effects or prevent the recurrence of TNBC of the skin. Patients should discuss their long-term care plan with their healthcare professional to ensure that they receive the appropriate care and support.
In conclusion, TNBC of the skin requires a comprehensive management plan that includes coping with side effects and follow-up and long-term care. Patients should work closely with their healthcare professional to develop a plan that meets their individual needs and provides the best possible outcomes.
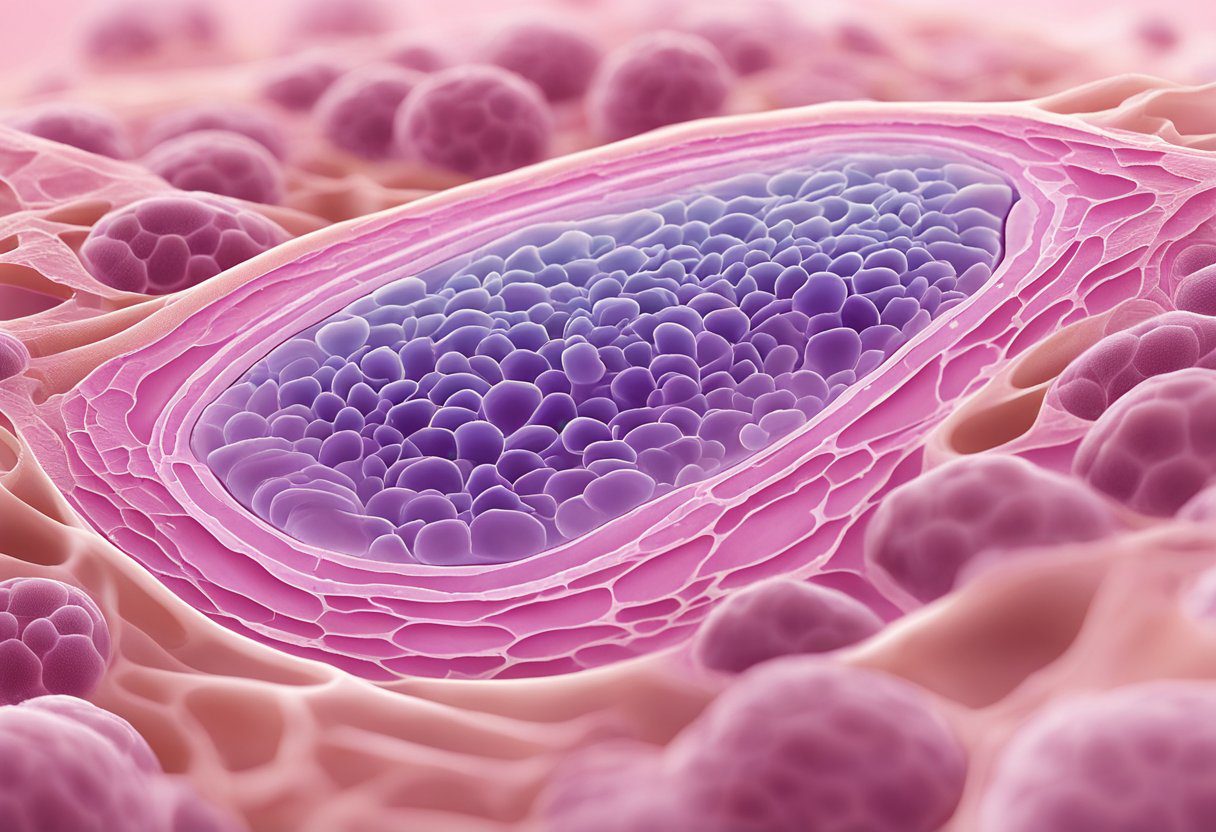
TNBC Skin Pictures
Skin manifestations of TNBC, particularly when the cancer has metastasized, can vary and may include:
-
- Nodules and Masses: Firm, often painless nodules or masses that can be felt under the skin. These may vary in size and can appear anywhere on the body but are more commonly found in areas close to the original breast cancer site.
-
- Inflammatory Breast Cancer (IBC): Though not exclusive to TNBC, inflammatory breast cancer is a rare and aggressive form. It can manifest as red, swollen, and tender skin over the breast, resembling an infection like mastitis. The skin may appear pitted or have a texture similar to an orange peel (peau d’orange). IBC requires immediate medical attention.
-
- Lymphedema: While not a direct skin manifestation, TNBC can cause lymphedema if it affects the lymphatic system, leading to swelling in the arms, legs, or other areas. The skin over the swollen area can feel tight and may become thicker or harder over time.
-
- Metastatic Skin Lesions: Rarely, TNBC can metastasize to the skin, leading to lesions that may look like nodules, ulcers, or rash-like areas. These lesions can be painful or itchy and might bleed or ooze.
-
- Carcinoma Erysipelatoides: This is a rare manifestation where the skin over the breast looks red and feels warm, mimicking erysipelas (a type of skin infection). It is caused by cancer cells blocking lymphatic vessels.
-
- Skin Changes from Treatment: Treatments for TNBC, including chemotherapy, radiation, and surgery, can also lead to skin changes. These may include rashes, hyperpigmentation, dryness, and sensitivity to sunlight.
TNBC skin pictures of all these skin manifestations can be found on the Internet. They are not presented here because of explicit content of images of TNBC and skin metastases.
Frequently Asked Questions
What are the common symptoms of skin metastasis in triple-negative breast cancer?
Skin metastasis in triple-negative breast cancer (TNBC) can present as rapidly growing nodules or as an inflammatory process that resembles a skin infection. According to a source, the most common symptoms of skin metastasis in TNBC include skin nodules, redness, swelling, and itching.
How does triple-negative breast cancer typically present on the skin?
Triple-negative breast cancer is known for its aggressive nature and higher chances of recurrence compared to other types of breast cancer. According to Healthline[9], TNBC can present on the skin as rapidly growing nodules or as an inflammatory process that resembles a skin infection. In some cases, TNBC can cause skin puckering, which is a sign of underlying cancer cells pulling on the skin’s connective tissue.
What are the latest treatment options for triple-negative breast cancer?
The treatment options for TNBC depend on the stage and extent of the cancer. According to Power[10], chemotherapy is a primary treatment method for TNBC skin metastasis. Other treatment options may include surgery, radiation therapy, and targeted therapy. However, research is ongoing to identify new and more effective treatments for TNBC.
What are the risk factors associated with developing triple-negative breast cancer?
The risk factors associated with developing TNBC include a family history of breast or ovarian cancer, being diagnosed at a younger age, and having a BRCA1 gene mutation. According to the American Cancer Society[4], African American women and Hispanic women are more likely to develop TNBC than white women.
What advancements have been made in treating triple-negative breast cancer?
Recent advancements in treating TNBC include the development of immunotherapy drugs that help the immune system recognize and attack cancer cells. According to MSD[11], clinical trials are ongoing to test the effectiveness of these drugs in treating TNBC. Additionally, research is ongoing to identify new biomarkers that can help predict the response to treatment and improve outcomes for TNBC patients.
How can skin puckering be related to triple-negative breast cancer?
Skin puckering, also known as skin tethering, can be a sign of underlying cancer cells pulling on the skin’s connective tissue. According to Breastcancer.org[12], skin puckering can be a symptom of TNBC, as well as other types of breast cancer. If you notice any changes in the appearance of your breast or skin, it is important to speak with a healthcare provider to determine the cause and receive appropriate treatment.
References
- Amazon.com : triple negative breast cancer shirt. https://amzn.to/4ai2wco Accessed November 6, 2025
- Amazon.com: In This Family No One Fights Alone Breast Cancer Awareness T-Shirt : Clothing, Shoes & Jewelry. https://amzn.to/3PBp0xj Accessed November 6, 2025
- Amazon.com : triple negative breast cancer bracelets. https://amzn.to/3TBLmB8 Accessed November 6, 2025
- 403 Forbidden. https://www.cancer.org/cancer/types/breast-cancer/about/types-of-breast-cancer/triple-negative.html Accessed November 6, 2025
- Case Series of Different Onset of Skin Metastasis According to the Breast Cancer Subtypes. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4022829/ Accessed November 6, 2025
- Triple-Negative Breast Cancer (TNBC). https://my.clevelandclinic.org/health/diseases/21756-triple-negative-breast-cancer-tnbc Accessed November 6, 2025
- Amazon.com : triple negative breast cancer apparel. https://amzn.to/4ad0WZp Accessed November 6, 2025
- Case report of long-term survival with metastatic triple-negative breast carcinoma: Treatment possibilities for metastatic disease. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6494386/ Accessed November 6, 2025
- Triple Negative Breast Cancer (TNBC): Symptoms and more. https://www.healthline.com/health/triple-negative-breast-cancer-symptoms Accessed November 6, 2025
- Inside Tnbc Skin. https://www.withpower.com/guides/inside-tnbc-skin Accessed November 6, 2025
- Page not found. https://www.msd.com/stories/triple-negative-breast-cancer-risks-signs-and-symptoms-and-diagnosis/ Accessed November 6, 2025
- Page not found. https://www.breastcancer.org/symptoms/types/recur_metast/puckering Accessed November 6, 2025

