Atherosclerosis is a condition where plaque builds up inside the arteries, making them hard and narrow. This can slow or block blood flow, leading to serious health problems. Understanding and managing atherosclerosis is crucial for preventing complications such as heart attacks and strokes.

Many factors can contribute to the development of atherosclerosis, like high cholesterol, high blood pressure, and smoking. Symptoms may not appear until an artery is significantly blocked, making early detection and lifestyle changes essential. Treatments range from medications to surgical procedures.
Preventing atherosclerosis involves adopting a heart-healthy lifestyle. Regular exercise, a balanced diet, and avoiding tobacco use can reduce the risk. Staying informed about atherosclerosis and its management is key to maintaining good health.
Key Takeaways
- Atherosclerosis involves plaque buildup in arteries.
- Early detection and lifestyle changes are crucial.
- Prevention includes exercise and a balanced diet.
Understanding Atherosclerosis
Atherosclerosis is a condition where plaque builds up inside the arteries, leading to reduced blood flow. This can result in serious health problems like heart attacks and strokes.
Definition and Basics
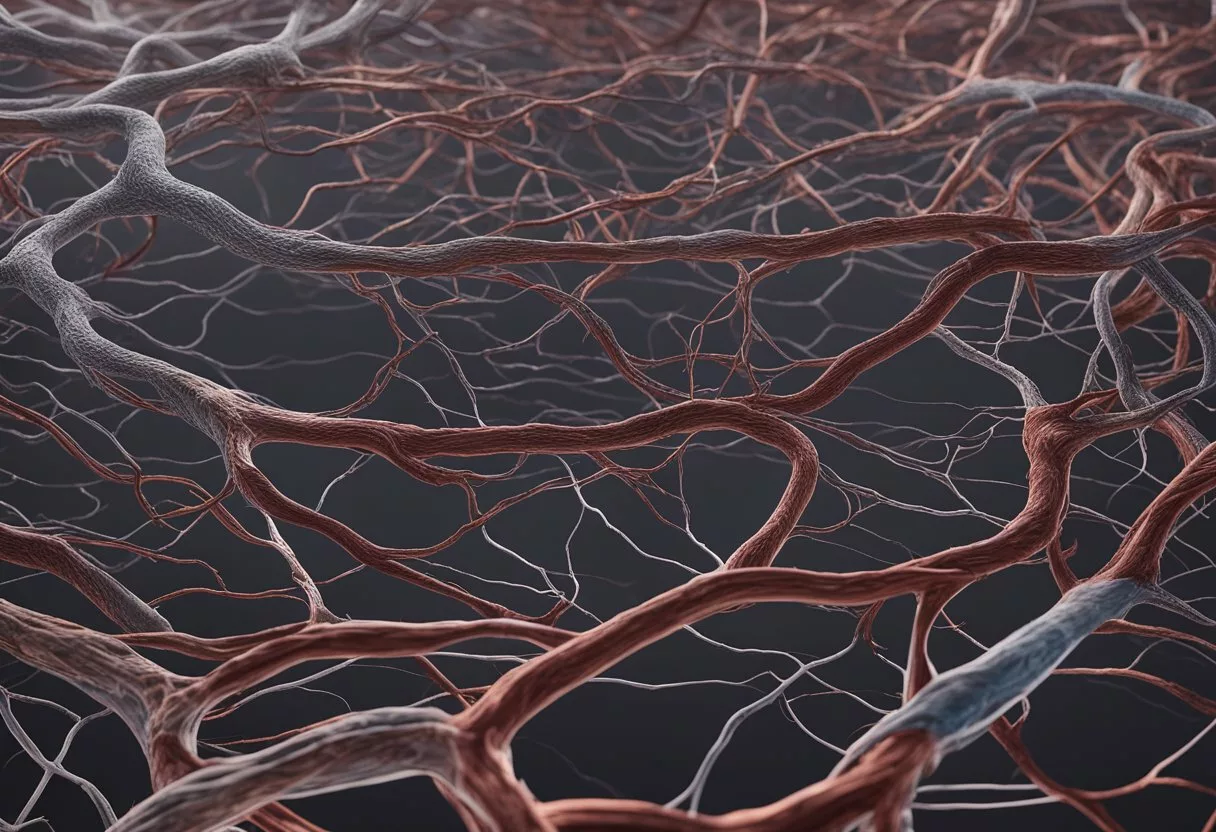
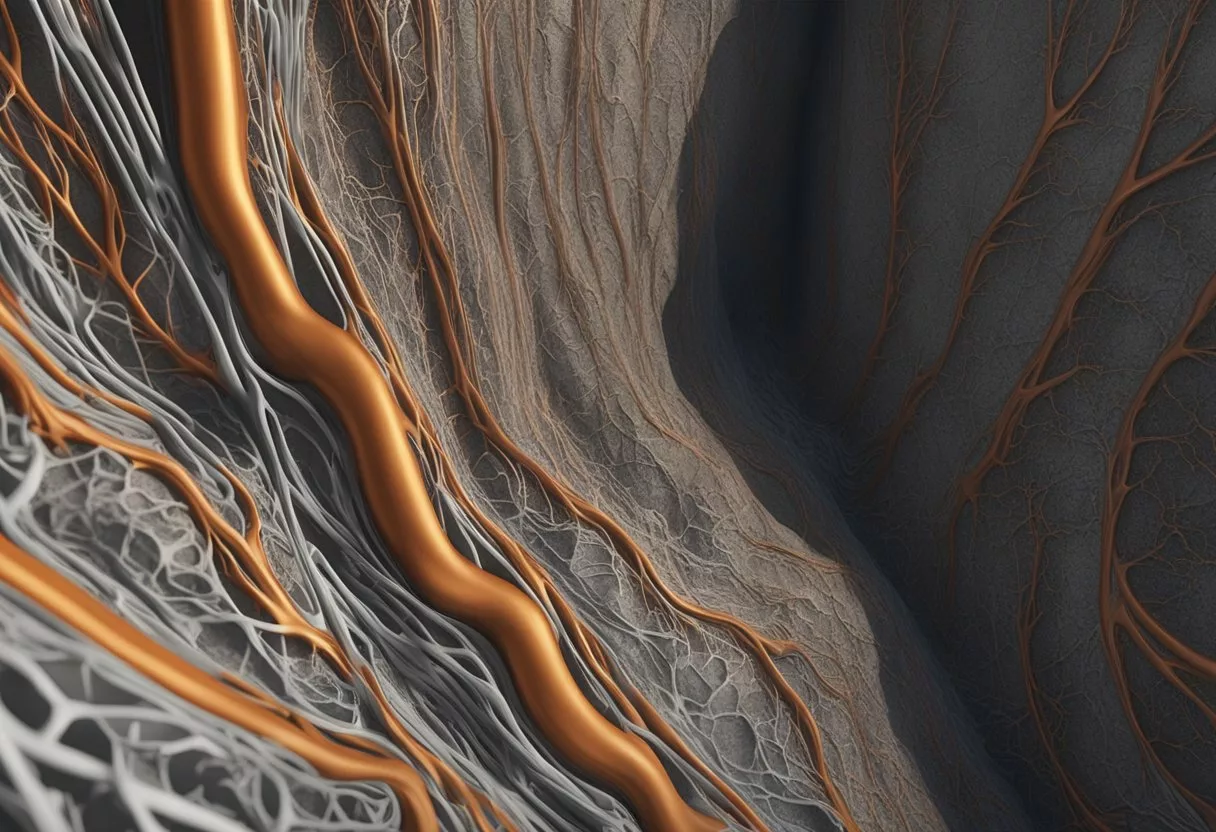
Atherosclerosis occurs when fatty materials, cholesterol, and other substances form plaque inside the arteries. Over time, this plaque can harden, a condition known as arteriosclerosis. This reduces or blocks blood flow, affecting the organs and tissues.
Healthy arteries are flexible and elastic, but atherosclerosis causes them to thicken and become stiff. As plaque accumulates, it makes the arteries narrower, increasing the risk of blood clots. This process can progress silently over many years before symptoms become noticeable.
Causes of Atherosclerosis
Several factors contribute to the development of atherosclerosis. High levels of cholesterol, particularly low-density lipoprotein (LDL), play a key role. LDL can enter the arterial walls and trigger inflammation.
Lifestyle factors such as poor diet, lack of exercise, smoking, and obesity significantly increase the risk. Genetic predispositions also contribute. Arteriosclerosis is often a result of this plaque buildup, leading to the hardening of arteries.
Chronic conditions like hypertension and diabetes accelerate the process. These conditions damage the inner layers of the arteries, making it easier for cholesterol and other substances to accumulate.
Pathophysiology
The pathophysiology of atherosclerosis involves several steps. Initially, damage to the endothelium, the inner lining of the artery, allows LDL cholesterol to penetrate the arterial wall. This LDL is then oxidized, leading to an inflammatory response.
Immune cells, particularly macrophages, migrate to the site of damage. They engulf the oxidized LDL, becoming foam cells and forming a fatty streak, the earliest sign of atherosclerosis.
Over time, these foam cells die, releasing their contents and thickening the vessel wall. Smooth muscle cells migrate to the area, contributing to the formation of a fibrous cap over the plaque. This cap can rupture, leading to the formation of a blood clot, which can block the artery completely, causing serious health issues such as heart attacks or strokes. This intricate process underscores the complexity of atherosclerosis development.
Risk Factors
Atherosclerosis is influenced by genetic factors, lifestyle choices, and various health conditions. These factors can increase the likelihood of plaque buildup in the arteries, leading to severe health issues like heart attack and stroke.
Genetic Influences
Family history plays a significant role in atherosclerosis. If a parent or sibling has had early heart disease, the risk of developing atherosclerosis increases. Genetics can affect how the body handles cholesterol and blood pressure, making some individuals more prone to plaque buildup.
Age is another critical factor. As people age, their arteries naturally lose elasticity, which can lead to hardening and thickening. Those over 45 years old assigned male at birth (AMAB) and 55 years old assigned female at birth (AFAB) are at higher risk. Genetic predisposition combined with aging significantly escalates the likelihood of developing atherosclerosis.
Lifestyle Choices
Smoking is a major contributor to atherosclerosis. It damages the inner lining of the arteries, facilitating plaque accumulation. Even exposure to secondhand smoke increases risk. Quitting smoking can significantly improve artery health.
Diet and physical activity are pivotal. Consuming foods high in saturated fats, trans fats, and cholesterol can lead to elevated cholesterol levels, while a lack of physical activity can contribute to obesity and raised blood pressure. Adopting a heart-healthy diet and regular exercise can mitigate these risks.
Stress also impacts lifestyle choices. Chronic stress may lead to behaviors like overeating, smoking, or lack of exercise, all of which increase cardiovascular risk. Managing stress through relaxation techniques or professional help can improve overall heart health.
Health Conditions
High blood pressure, or hypertension, is a significant risk factor for atherosclerosis. Over time, high blood pressure damages the artery walls, making them more susceptible to plaque buildup. Managing blood pressure through lifestyle changes and medication is crucial.
Diabetes, particularly type 2 diabetes, raises the risk of atherosclerosis. High blood sugar levels can damage blood vessels, accelerating the process of plaque formation. Effective management of diabetes is essential to reduce this risk.
Obesity is linked to several atherosclerosis risk factors, including high blood pressure, diabetes, and unhealthy blood lipid levels. Reducing weight through a balanced diet and regular physical activity can significantly lower these risks.
These health conditions underscore the importance of medical intervention and lifestyle adjustments in managing atherosclerosis risk.
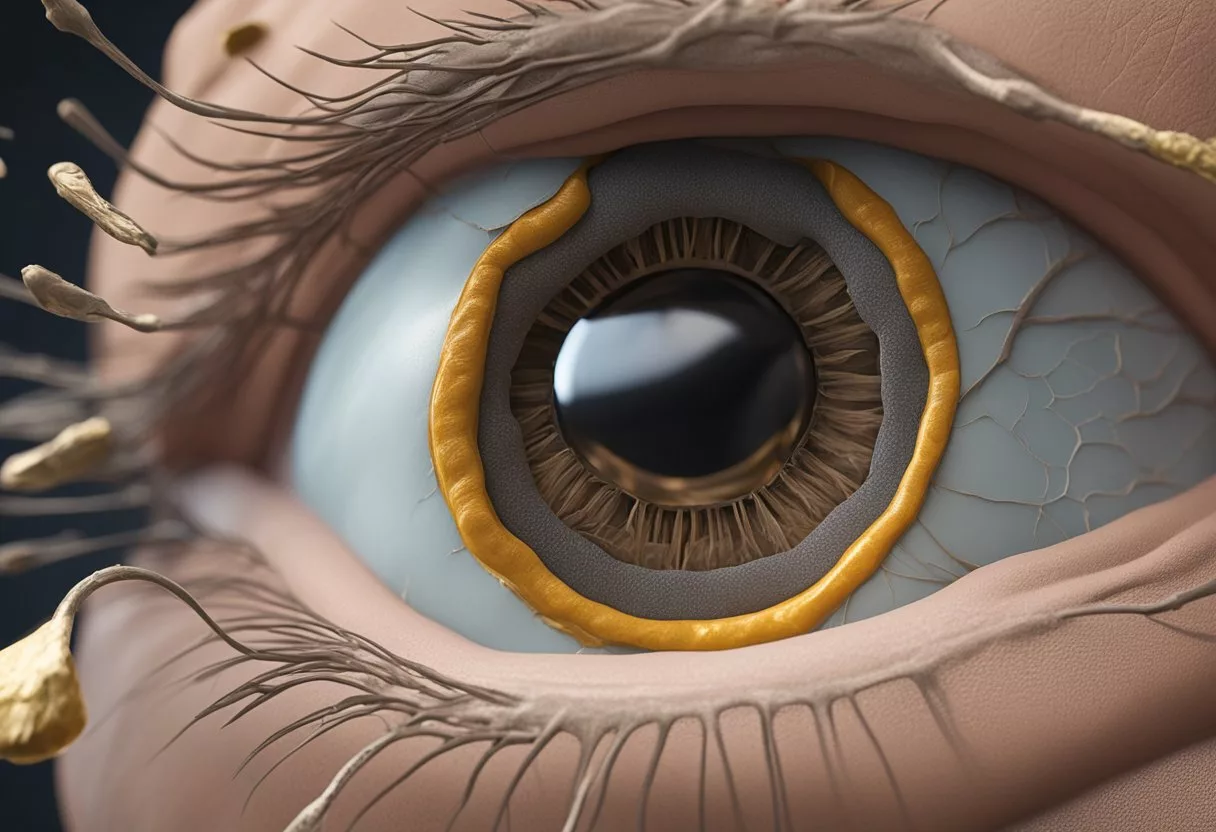
Symptoms and Detection
Atherosclerosis can be difficult to detect early because it often progresses without noticeable symptoms. Knowing the early indicators, advanced symptoms, and diagnostic procedures can be life-saving.
Early Indicators
Early indicators of atherosclerosis may not be obvious. Some people may experience chest pain (angina) or shortness of breath during physical activity. Fatigue and weakness may also occur. Another sign can be pain in the legs during walking, indicating peripheral artery disease. Symptoms like numbness or weakness in the limbs may suggest reduced blood flow. These signs should prompt a visit to the doctor for further investigation.
Advanced Symptoms
As atherosclerosis advances, symptoms become more apparent and severe. Chest pain becomes more frequent and severe. Increased shortness of breath is noticeable even during minimal physical activities. Pain in the limbs may become constant. Additionally, the person might experience symptoms of a heart attack or stroke, such as intense chest pain, difficulty speaking, or sudden weakness on one side of the body. Immediate medical attention is crucial at this stage.
Diagnostic Procedures
Diagnosis of atherosclerosis involves several medical tests. A physical exam is often the first step, where a doctor checks for weak pulses or abnormal sounds in the arteries. Blood tests can detect high cholesterol or inflammation markers. An electrocardiogram (ECG) can show heart problems. The ankle-brachial index measures blood pressure in the ankle and compares it to the arm to find blockages. A Doppler ultrasound evaluates blood flow through the vessels. For detailed imaging, a magnetic resonance angiography (MRA) can visualize artery blockages.
For more detailed information on early indicators, visit WebMD. For details on diagnostic procedures, refer to Cleveland Clinic.
Complications of Atherosclerosis
Atherosclerosis can lead to serious health problems by restricting blood flow. The most common complications include heart-related events, peripheral artery disease, and cerebrovascular accidents.
Heart-Related Events
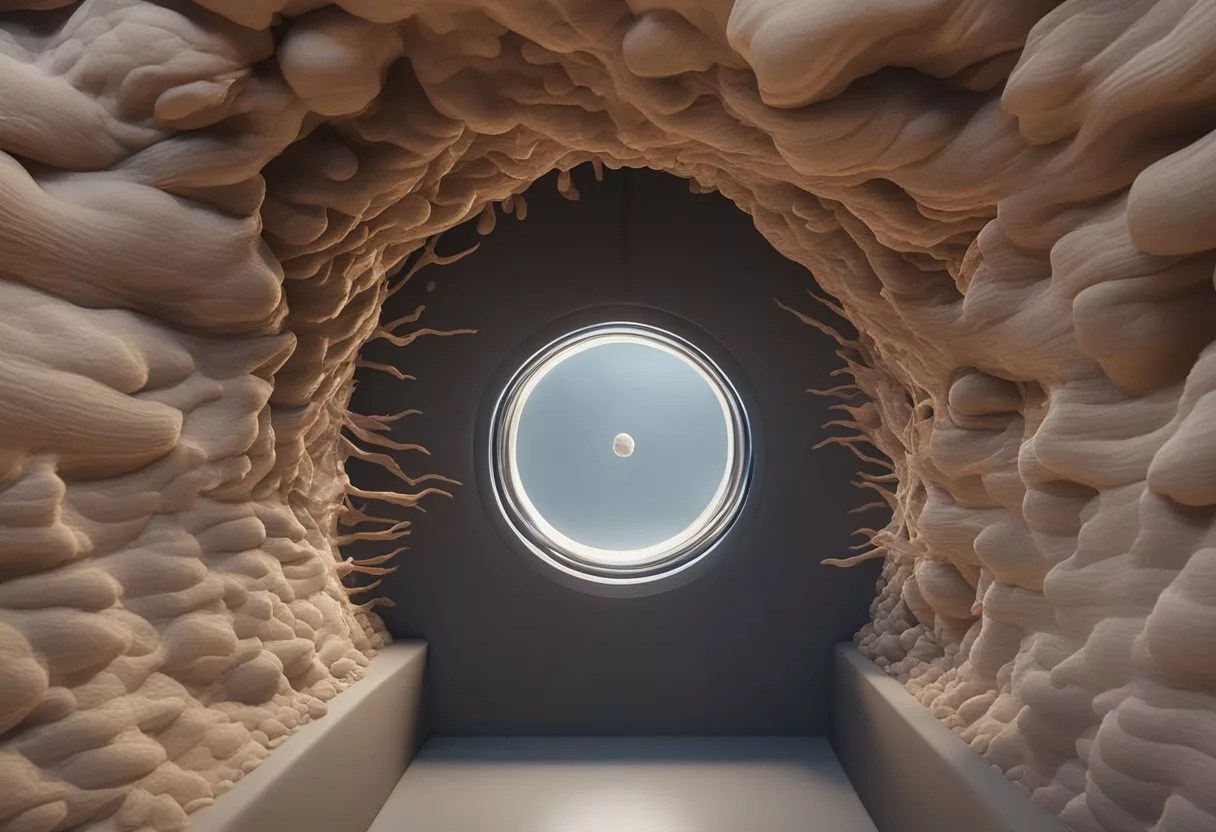
When the coronary arteries become narrowed or blocked by plaque, it can lead to coronary artery disease. This condition can result in chest pain (angina), heart attacks, and even heart failure. Importantly, a heart attack occurs when a blood clot completely obstructs blood flow to the heart muscle, causing tissue damage.
A blood clot can form on the surface of ruptured plaque. This restricts oxygenated blood from reaching vital areas, risking coronary heart disease complications. Aneurysms, bulges in the artery walls, may also develop, posing further risks.
Peripheral Artery Disease
Atherosclerosis can also affect arteries in the legs and arms, known as peripheral artery disease (PAD). Decreased blood flow to the limbs can cause pain, numbness, and increased risk of infections.
PAD increases the risk of developing infections where the body heals more slowly. There is also a higher chance of blood clots forming in the narrowed arteries. In severe cases, lack of blood flow can lead to tissue death and amputation.
Cerebrovascular Accidents
Plaque buildup in the carotid arteries, known as carotid artery disease, can reduce blood flow to the brain and lead to stroke. A stroke occurs when a blood clot or a ruptured plaque blocks a cerebral artery, cutting off oxygen to part of the brain.
A transient ischemic attack (TIA), often called a mini-stroke, is a temporary period of reduced blood flow. While it does not cause permanent damage, it is often a warning sign of potential future strokes. Additionally, chronic kidney disease can arise from restricted blood flow to the kidneys.
For more detailed information, you can visit the Cleveland Clinic and Mayo Clinic.
Treatment and Management

Treatment and management of atherosclerosis involve lifestyle changes, medications, and sometimes surgical interventions. These measures aim to reduce risk factors, improve blood flow, and prevent complications such as heart attacks or strokes.
Lifestyle Modifications
Lifestyle modifications are crucial in managing atherosclerosis. Regular exercise like walking can improve cardiovascular health by reducing blood pressure and cholesterol levels. Exercise also helps to maintain a healthy weight, which is essential for heart health.
A healthy diet rich in fruits, vegetables, whole grains, and lean proteins can also greatly impact disease management. It is important to limit saturated fats, trans fats, and added sugars.
Quitting smoking is another essential step, as smoking damages artery walls and accelerates plaque buildup. Reducing alcohol intake can also help manage symptoms.
Medication
Medications are often prescribed to lower cholesterol, control blood pressure, and prevent blood clots. Statins are commonly used to lower LDL (“bad”) cholesterol and stabilize plaque.
Aspirin may be recommended in low doses to reduce the risk of heart attacks by preventing blood clots. Other medications like niacin, fibrates, and bile acid sequestrants may also be used to manage cholesterol levels.
In addition, blood pressure medications such as beta-blockers, ACE inhibitors, or calcium channel blockers help keep hypertension under control, reducing the burden on the arteries.
Surgical Interventions
Surgical interventions may be necessary when lifestyle changes and medications are not enough. Angioplasty is a common procedure where a balloon is used to open narrowed arteries, often with a stent placement to keep them open.
An endarterectomy is another surgical option that involves removing plaque from the artery walls, improving blood flow.
In severe cases, bypass surgery may be performed to redirect blood flow around blocked arteries. These procedures can significantly reduce symptoms and improve quality of life for those with advanced atherosclerosis.
These strategies together can play a vital role in managing atherosclerosis, reducing complications, and promoting heart health.
Prevention Strategies

Preventing atherosclerosis involves significant lifestyle choices, focusing on healthy eating, regular exercise, and consistent health check-ups. This can reduce the risk of atherosclerosis and improve overall well-being.
Dietary Approaches
A healthy diet plays a crucial role in preventing atherosclerosis. Emphasizing foods low in saturated fats and sugar is critical. Saturated fats should be replaced with unsaturated fats found in fish, nuts, and oils. Eating fish rich in omega-3 fatty acids, such as salmon and mackerel, can be beneficial for heart health.
Including plenty of fruits and vegetables is fundamental, as they are rich in antioxidants and fiber, which help reduce cholesterol levels. Whole grains, like oats and brown rice, should replace refined grains. Quitting smoking also improves dietary choices and further reduces risks related to atherosclerosis.
Physical Activity Recommendations
Regular exercise is essential in preventing atherosclerosis. A mix of aerobic exercises, such as walking, cycling, and swimming, helps improve cardiovascular fitness and vascular health. Routine physical activity increases oxygen delivery to tissues, supports heart function, and helps control weight, reducing strain on the arteries.
Aim for at least 150 minutes of moderate exercise or 75 minutes of vigorous activity each week. Including muscle-strengthening activities twice a week can also be beneficial. Physical activity helps control hypertension, maintain a healthy weight, and reduce blood cholesterol levels.
Regular Health Screenings
Frequent health screenings enable early detection and management of risk factors related to atherosclerosis. Regularly checking blood pressure, cholesterol levels, and blood sugar levels can identify potential issues before they become severe. Health screenings are particularly important for individuals with a family history of heart disease.
Stress tests can evaluate the heart’s reaction to physical activity, identifying any hidden issues. Regular consultations with healthcare providers are crucial in maintaining heart health. They can offer customized advice based on individual health profiles, promoting effective prevention strategies. Regular health screenings help ensure timely intervention and improved heart health outcomes.
Emerging Research and Innovations

Recent advances in the treatment of atherosclerosis focus on genetic research and new treatment modalities. These innovations aim to tackle key areas like lipoprotein levels, inflammation, and plaque management, offering promising developments in combating cardiovascular diseases.
Genetic Research
Genetic research is making significant strides in understanding atherosclerosis. Scientists are exploring the role of genes in the development of this disease. By identifying genetic mutations that increase the risk of atherosclerosis, researchers hope to create targeted therapies.
One promising area is the use of mRNA technology to edit or encode desired genes. This approach could help reduce harmful lipoproteins that contribute to plaque formation. Additionally, miRNA recognition sequences are being investigated for their ability to allow cell-selective expression of therapeutics.
These genetic innovations aim to address the root causes of atherosclerosis by targeting specific genetic pathways. The goal is to develop personalized treatments that can prevent or reduce plaque buildup and related complications.
New Treatment Modalities
New treatments are focusing on coupling diagnostics with therapeutics to improve outcomes for patients with atherosclerotic cardiovascular disease. Combining imaging techniques with drug delivery systems allows for precise targeting of atherosclerotic plaques.
Emerging therapies include the use of C-reactive protein inhibitors to reduce inflammation in the arterial walls. This chronic inflammation contributes to the progression of the disease.
Furthermore, there is ongoing research into the use of fibrin-modulating agents to stabilize plaques and prevent rupture. Researchers are also developing drugs to regulate the immune system’s response to arterial damage, which is crucial in preventing the formation of new plaques.
These new modalities aim to provide comprehensive solutions that address multiple aspects of atherosclerosis, from diagnosis to treatment, improving patient care and outcomes.
Frequently Asked Questions
Atherosclerosis is a serious condition that involves the buildup of plaque in the arteries. It can lead to various health problems. Understanding its symptoms, treatments, and causes is crucial.
What are the common symptoms of atherosclerosis?
Early stages of atherosclerosis might not show symptoms. When symptoms appear, they often include chest pain (angina), shortness of breath, fatigue, and pain in the limbs. These symptoms occur because of reduced blood flow to the heart or other parts of the body.
How is atherosclerosis treated?
Treatments for atherosclerosis include lifestyle changes, medications, and medical procedures. Lifestyle changes might involve a healthier diet, regular exercise, and quitting smoking. Medications can help lower cholesterol and blood pressure. In more severe cases, procedures like angioplasty or surgery might be required.
What are the primary causes of atherosclerosis?
The primary causes of atherosclerosis are high cholesterol, high blood pressure, smoking, and diabetes. These factors contribute to plaque buildup in the arteries. Poor diet and lack of exercise are also significant contributors.
What distinguishes atherosclerosis from arteriosclerosis?
Atherosclerosis and arteriosclerosis are related but different conditions. Atherosclerosis specifically involves the buildup of fatty plaques inside the arteries. Arteriosclerosis refers to the general hardening and thickening of the arteries, which can happen for various reasons, including aging.
How is atherosclerosis diagnosed?
Atherosclerosis is diagnosed through various tests. Common tests include blood tests to check cholesterol levels, electrocardiogram (EKG) to monitor heart activity, and imaging tests like CT scans to view the arteries. A heart scan might show calcium deposits in the artery walls.
What factors increase the risk of developing atherosclerosis?
Risk factors for developing atherosclerosis include high cholesterol, high blood pressure, smoking, obesity, diabetes, and a sedentary lifestyle. Family history and age also play important roles. Men are generally at higher risk than women, but women’s risk increases after menopause.
For more detailed information, you can refer to resources like the Mayo Clinic and CardioSmart.