Heart disease is a leading cause of death globally. With various types and numerous contributing factors, understanding heart disease is crucial for prevention and treatment. Heart disease encompasses conditions such as coronary artery disease, heart valve problems, and heart failure. Each type can manifest through different symptoms, including chest pain, shortness of breath, and even pain in the neck or back.
Many risk factors contribute to heart disease, including high blood pressure, high cholesterol, smoking, and a sedentary lifestyle. Early detection through regular check-ups and recognizing symptoms can significantly improve the outcomes for those affected. Lifestyle changes, such as maintaining a healthy diet, regular exercise, and avoiding tobacco, are vital preventive measures.
Treatment options vary depending on the type and severity of the heart disease. They may range from medications and lifestyle adjustments to more invasive procedures like angioplasty or surgery. Understanding these aspects can help individuals take proactive steps towards maintaining their heart health and seeking timely medical intervention.
Key Takeaways
- Heart disease includes conditions like coronary artery disease and heart valve problems.
- Risk factors include high blood pressure, high cholesterol, smoking, and inactivity.
- Treatment ranges from lifestyle changes and medications to surgical procedures.
Understanding Heart Disease

Heart disease encompasses various heart conditions that lead to problems with the cardiovascular system. These conditions can affect the heart’s structure, function, or its blood vessels.
Defining Heart Disease and Its Types
Heart disease refers to multiple diseases related to the heart and blood vessels. Common types include Coronary Artery Disease (CAD), Heart Failure, Arrhythmia, Cardiomyopathy, Congenital Heart Disease, and Heart Valve Disease.
Coronary Artery Disease involves the buildup of plaque in the arteries, reducing blood flow. Heart Failure occurs when the heart can’t pump blood effectively. Arrhythmias are irregular heartbeats. Cardiomyopathy is a disease of the heart muscle. Congenital Heart Disease includes structural heart problems present at birth. Heart Valve Disease affects how valves function to regulate blood flow.
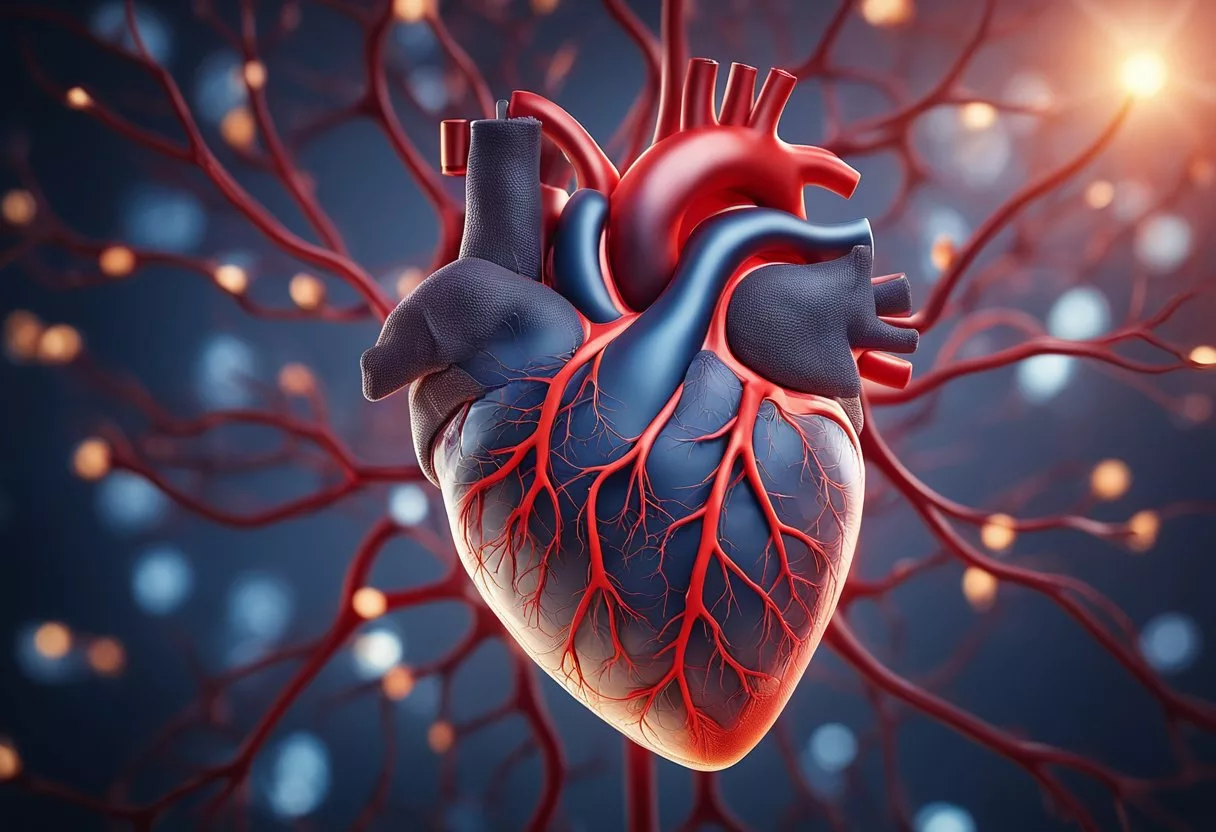
The Anatomy of the Heart
The heart is a muscular organ located in the chest, responsible for pumping blood throughout the body. It has four chambers: the left atrium, right atrium, left ventricle, and right ventricle.
Blood enters the atria and is pumped into the ventricles. The heart valves ensure one-way blood flow through these chambers. The mitral and tricuspid valves control blood flow from the atria to the ventricles. The aortic and pulmonary valves regulate blood flow out of the ventricles. The heart’s function depends on coordinated contractions controlled by electrical signals.
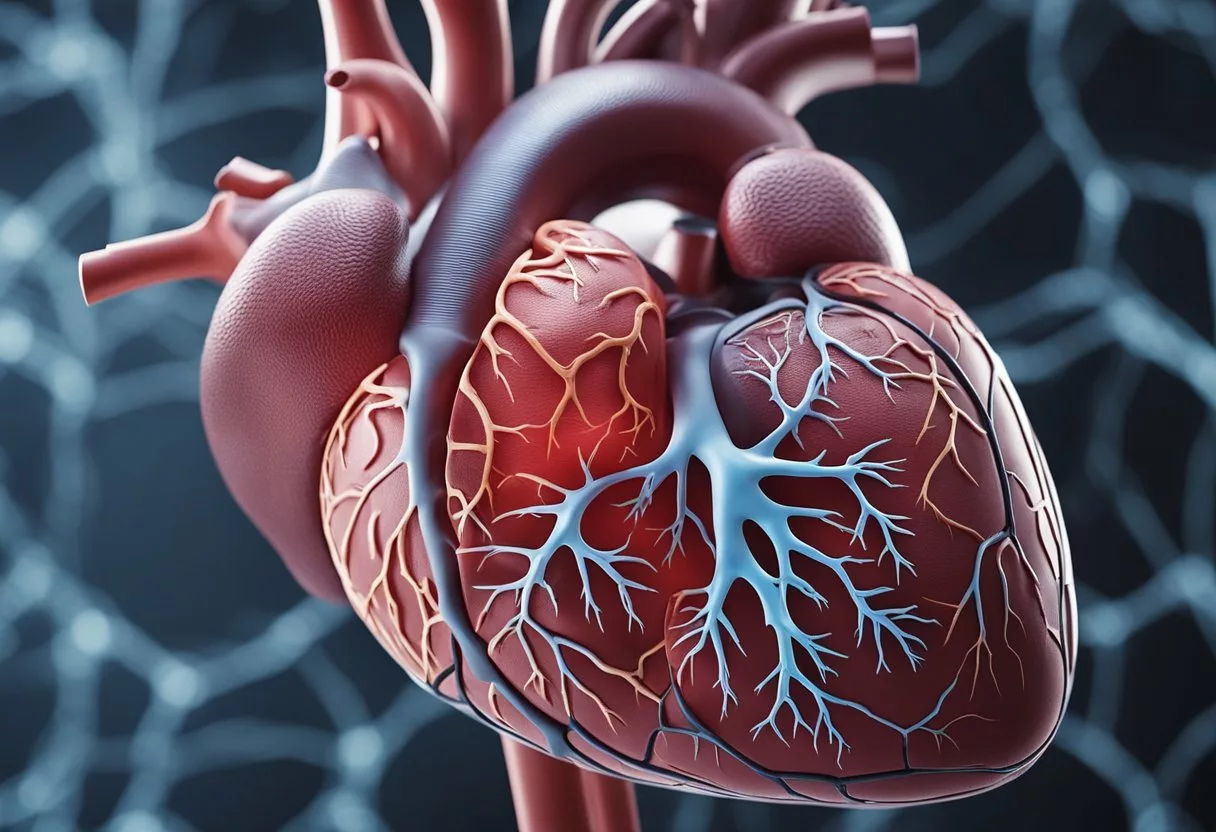
Common Types of Heart Diseases
Coronary Artery Disease (CAD) is the most prevalent. It results from blocked arteries due to plaque buildup and can lead to a heart attack.
Heart Failure means the heart doesn’t pump blood well, causing fatigue and breathlessness. Arrhythmias include irregular heartbeats that can disrupt normal blood flow. Cardiomyopathy affects the heart muscle, impairing its ability to pump.
Congenital Heart Disease includes structural issues present from birth, such as holes in the heart or malformed valves. Heart Valve Disease involves damage or defects in one of the four heart valves, which can cause either narrowing (stenosis) or leaking (regurgitation).
Understanding these types is essential for diagnosing and treating heart conditions effectively.
Causes and Risk Factors
Various factors contribute to heart disease. These factors can be categorized into lifestyle and environmental influences, genetic predispositions, and other medical conditions.
Lifestyle and Environmental Factors
Lifestyle and environmental aspects play a significant role in the development of heart disease. Smoking is a major risk factor due to its impact on blood vessels and heart function. People who smoke are more likely to develop conditions such as coronary artery disease.
Diet and lack of physical activity also contribute to heart disease. Consuming high amounts of saturated fats, trans fats, and cholesterol can lead to plaque build-up in arteries.
Excessive alcohol consumption can raise blood pressure and triglyceride levels. People with sedentary lifestyles are more prone to obesity and high blood pressure, both of which increase heart disease risk.
Stress is another factor. Chronic stress can lead to harmful habits like overeating, smoking, and alcohol abuse, which further impact heart health.
Genetics and Family History
Heart disease often runs in families, suggesting a genetic component. If a person has a family history of heart disease, they are more likely to develop it themselves.
Inherited conditions, such as familial hypercholesterolemia, can lead to high cholesterol levels from a young age. This significantly increases the risk of heart disease.
Genetics can also influence how the body processes fats and how much cholesterol and triglycerides circulate in the blood.
Age is another genetic factor. As people age, their risk of heart disease increases. Men are at greater risk after 45, and women are at greater risk after 55.
Other Medical Conditions
Certain medical conditions can also raise the likelihood of heart disease. High blood pressure forces the heart to work harder, causing the heart muscle to thicken and become stiff.
Diabetes is a significant risk factor due to its association with increased blood sugar levels, which can damage blood vessels.
Obesity is closely linked to heart disease. Excess body weight typically increases the risk of high blood pressure, high cholesterol, and diabetes.
Other conditions like autoimmune diseases and chronic kidney disease can also elevate the risk of heart disease. Managing these conditions through medication and lifestyle changes is crucial in reducing heart disease risk.
Symptoms and Early Detection
Recognizing and diagnosing heart disease early can greatly improve treatment outcomes. It is important to understand the symptoms and the diagnostic tests that help identify heart conditions.
Recognizing Common Symptoms
Common symptoms of heart disease include chest pain, which often feels like tightness, squeezing, or pressure. Shortness of breath can occur during activity or rest. Some people may experience dizziness or feel lightheaded.
Fatigue is another symptom, where even simple tasks can cause extreme tiredness. Palpitations or feeling like the heart is racing or skipping beats can also be a sign. Other symptoms include nausea, swelling in legs or abdomen, and pain in the neck, jaw, or back.
Symptoms can vary depending on the type of heart disease. Coronary artery disease might cause pain in the arm, neck, or jaw, while valve problems might result in fatigue and palpitations.
Diagnostic Tests and Procedures
Electrocardiograms (ECG) are often used to detect irregular heart rhythms. An echocardiogram uses sound waves to create images of the heart, helping doctors see its structure and function.
Blood tests can reveal markers that indicate heart damage or risk. A stress test monitors the heart’s response to physical activity, showing how well the heart works under stress.
Angiograms involve using dye and X-rays to visualize blood flow in the heart arteries, helping identify blockages. This procedure is particularly useful for diagnosing coronary artery disease.
Early detection through these tests can significantly improve the management and treatment of heart disease, potentially preventing serious complications.
Preventive Measures
Preventing heart disease involves a combination of lifestyle changes and healthy habits. Key areas of focus include quitting smoking, maintaining a balanced diet, staying active, and managing stress.
Lifestyle Modifications
Quitting smoking is one of the most significant changes someone can make to improve their heart health. Smoking damages the blood vessels and increases the risk of heart disease. Avoiding secondhand smoke is also important.
Reducing alcohol intake can lower the risk of heart disease. Drinking too much alcohol can raise blood pressure and contribute to weight gain. Limiting alcohol consumption to moderate levels is recommended.
Stress management is another vital aspect. High stress levels can increase blood pressure and lead to unhealthy behaviors, such as overeating or smoking. Techniques like meditation, yoga, and deep breathing exercises can help keep stress levels in check.
Nutrition and Diet
A healthy diet rich in fruits, vegetables, whole grains, and lean proteins can significantly reduce the risk of heart disease. Avoiding foods high in saturated fats, trans fats, and cholesterol is crucial for maintaining heart health.
Consuming foods high in fiber helps lower cholesterol levels. Diets that include plenty of fresh fruits and vegetables provide essential vitamins and nutrients that support heart health. Limiting sodium intake helps keep blood pressure in a healthy range.
Managing diabetes through a careful diet can prevent complications that increase heart disease risk. Monitoring blood sugar levels and following a doctor’s recommendations regarding diet and medication is important.
Regular Exercise and Physical Activity
Regular exercise helps maintain a healthy weight and reduces stress. Activities like walking, running, cycling, and swimming improve cardiovascular health. Aim for at least 150 minutes of moderate exercise each week, or 75 minutes of vigorous activity.
Incorporating physical activity into daily routines, such as taking the stairs instead of the elevator or walking during breaks, can make a significant difference.
Getting good sleep also supports heart health. Poor sleep can contribute to high blood pressure, obesity, and diabetes, all of which are risk factors for heart disease.
In summary, making lifestyle changes, following a balanced diet, and engaging in regular physical activity are effective strategies for preventing heart disease.
Treatment Options
There are several ways to manage heart disease. These include medicines, surgical procedures, and non-surgical interventions. Each treatment plan depends on the type and severity of the condition.
Medications and Drug Therapy
Medications play a key role in treating heart disease. Statins lower bad LDL cholesterol, which helps reduce plaque buildup. Common statins include atorvastatin and simvastatin. Beta-blockers help slow down the heart rate and lower blood pressure, reducing the heart’s workload. Examples are metoprolol and carvedilol.
ACE inhibitors relax blood vessels, making it easier for the heart to pump blood. Medications like lisinopril and enalapril are often used. Blood thinners like aspirin prevent blood clots from forming, which can help prevent heart attacks and strokes. It’s important to follow the healthcare provider’s instructions when taking these medicines to avoid side effects.
Interventional Procedures
Interventional procedures are less invasive than surgery and are often used to treat blockages in the heart’s arteries. Angioplasty involves inflating a small balloon inside the artery to widen it. Frequently, a stent is placed in the artery to keep it open.
Another procedure is Coronary Artery Bypass Surgery, where a healthy blood vessel is taken from another part of the body and used to bypass a blocked artery. These procedures aim to improve blood flow to the heart, reduce symptoms, and prevent heart attacks.
Surgical Treatments
When medications and interventional procedures are not enough, surgery may be required. One common surgical treatment is bypass surgery, specifically Coronary Artery Bypass Surgery (CABG). This surgery uses a blood vessel from another part of the body to create a new path for blood to flow around a blocked artery.
Heart valve surgery repairs or replaces damaged heart valves to ensure proper blood flow through the heart. For severe heart failure, a heart transplant might be necessary. These surgeries are major procedures and usually require extended recovery times, but can significantly improve quality of life and longevity.
Living with Heart Disease
Managing heart disease requires a combination of daily lifestyle changes, medication adherence, and ongoing support. Individuals often need to navigate additional chronic conditions and find effective support systems to improve their quality of life.
Day-to-Day Management
Daily management includes adhering to medication schedules, maintaining a heart-healthy diet, and engaging in regular physical activity. Medications such as beta-blockers, ACE inhibitors, and statins are commonly prescribed. Diet should emphasize fruits, vegetables, whole grains, and lean proteins like fish and chicken.
Regular exercise, as recommended by healthcare providers, can improve cardiovascular health. Patients should also monitor symptoms like chest pain and shortness of breath and schedule regular medical appointments to track their condition.
Key Points:
- Medications: Take as prescribed.
- Diet: Include heart-healthy foods.
- Exercise: Follow doctor’s guidelines.
- Monitoring: Keep track of symptoms.
Chronic Conditions and Comorbidities
People with heart disease often have other chronic conditions, such as diabetes or hypertension, which can complicate management. It’s crucial to control these conditions through medication, diet, and regular check-ups.
Doctors may adjust treatment plans to address multiple conditions efficiently. Careful coordination between different specialists ensures comprehensive care. Managing these comorbidities effectively can prevent complications and improve overall health outcomes.
Key Points:
- Diabetes: Monitor blood sugar levels.
- Hypertension: Keep track of blood pressure.
- Coordination: Work with multiple specialists.
- Treatment Plans: Adjust as needed.
Support Systems and Rehabilitation
Support from family, friends, and healthcare providers can significantly impact the well-being of individuals with heart disease. Cardiac rehabilitation programs offer structured support, including exercise training, education on heart-healthy living, and counseling services.
These programs help patients recover and reduce the risk of future heart problems. Emotional support is equally important; joining support groups or seeking therapy can help manage the psychological impact of heart disease.
Key Points:
- Family and Friends: Provide emotional and practical support.
- Cardiac Rehabilitation: Participate in structured programs.
- Support Groups: Join for shared experiences.
- Counseling: Address emotional health.
Cardiac Events and Emergencies

Cardiac events require immediate attention to prevent serious harm. Recognizing signs and providing timely responses can make a vital difference in outcomes.
Recognizing a Heart Attack
Heart attacks, or myocardial infarctions, happen when blood flow to the heart is blocked. Symptoms include chest pain, which may feel like pressure or squeezing. Pain can spread to the arms, back, neck, or jaw. Shortness of breath, cold sweats, and nausea are also common.
Prompt recognition and getting help quickly are crucial. Calling 911 and chewing an aspirin can save lives. While waiting for emergency services, keeping the individual calm and in a comfortable position is important.
Responding to a Stroke
Strokes occur when blood supply to the brain is interrupted. Recognizing the FAST signs is key:
- Face drooping
- Arm weakness
- Speech difficulties
- Time to call 911
Other symptoms include sudden confusion, trouble seeing, and severe headache. Immediate medical attention is required. Getting the person to a hospital quickly can greatly improve their chances of recovery. Emergency treatments can restore blood flow to the brain.
Managing Cardiac Arrest
Cardiac arrest occurs when the heart suddenly stops beating. Unlike heart attacks, there are often no warning signs. If a person collapses and is unresponsive or not breathing normally, immediate action is required.
Call 911 and start CPR immediately. Push hard and fast in the center of the chest (100-120 compressions per minute). If available, use an automatic external defibrillator (AED) as soon as possible. Early defibrillation and continuous CPR can significantly increase the chances of survival.
Innovations in Cardiology
Recent advancements have brought significant changes in the prevention and treatment of heart disease. Key developments include minimally invasive procedures and promising new therapies.
Advancements in Heart Disease Treatment
One of the major breakthroughs is the Transcatheter Aortic Valve Replacement (TAVR). This procedure treats aortic valve stenosis without open-heart surgery, reducing recovery time. It’s particularly beneficial for patients who are not candidates for traditional surgery.
Another innovation is in gene therapy, which offers potential for treating genetic causes of heart disease. This involves altering genes to correct abnormalities or introducing new genes to combat disease. Research is ongoing, but early results are promising.
Regenerative medicine is also playing a significant role. Scientists are exploring ways to repair or replace damaged heart tissue using stem cells. This could revolutionize treatments for heart failure by regenerating heart muscle instead of relying solely on medications.
Emerging Research and Therapies
In the realm of research, new findings are establishing links between childhood risk factors and future heart disease. Studies have shown that early life factors like obesity and smoking can lead to cardiovascular events later in life. This highlights the importance of early prevention strategies.
Digital health technologies are evolving rapidly. Wearable devices and mobile apps now help monitor heart health in real-time, providing valuable data to both patients and doctors. These technologies are helping improve diagnosis and management of heart conditions.
Moreover, new medications are being developed to target specific pathways in heart disease. These drugs offer more tailored and effective treatment options, potentially leading to better outcomes for patients.
The Role of Healthcare Providers

Healthcare providers play a critical role in diagnosing, managing, and treating heart disease. They offer specialized medical advice and ensure patients receive the necessary care to improve heart health and manage symptoms effectively.
Primary Care and Cardiology Specialists
Primary care providers are often the first to identify potential heart issues. They conduct initial assessments and check for risk factors such as high blood pressure, diabetes, and family history.
If heart disease is suspected, they may refer patients to cardiologists. Cardiologists specialize in diagnosing and treating heart conditions. They perform thorough examinations, including ECGs and imaging tests, to determine the precise nature of the heart problem. They also develop comprehensive treatment plans, which may involve medications, lifestyle changes, or surgeries.
Having both primary care and cardiology specialists involved ensures that patients receive holistic care tailored to their specific needs. This coordination between healthcare providers is essential in managing heart diseases effectively.
Preparing for Your Doctor’s Appointment
Preparing for a heart-related appointment can help make the visit more productive. Patients should prepare a list of symptoms, including their duration and any triggers. It can also be helpful to write down questions about their condition or treatment options.
Bringing a list of all current medications is essential, as some drugs can interact with heart medications. Knowing your family medical history, especially concerning heart disease, can provide valuable context for the healthcare provider.
Patients should be ready for potential tests, such as blood tests or imaging scans. Being informed and organized allows the healthcare provider to make a more accurate diagnosis and develop an effective treatment plan. Clear communication between patients and doctors is key to managing heart health.
Community and Resources

Accessible resources and support communities can make a significant difference for individuals managing heart disease. Effective support groups provide emotional aid, while online tools offer valuable educational resources.
Support Groups and Education
Community support groups offer a safe space for individuals to share experiences and advice. These groups can be found through local hospitals, community centers, and online platforms. They provide a sense of belonging and can reduce feelings of isolation.
Educational resources are vital for those living with heart disease. Organizations like the American Heart Association provide workshops, seminars, and pamphlets on managing the condition. Such resources help patients understand symptoms and treatments better.
Many hospitals also offer patient education programs. These programs include diet and exercise plans tailored to individual needs, as well as information on medication management.
Online Resources and Tools
Online tools and resources offer convenient access to information and support. Websites like CDC and Verywell Health provide detailed info on various heart conditions.
Various apps track heart health metrics like blood pressure and heart rate. These digital tools help patients monitor their health and stay connected with healthcare providers.
Forums and online communities, such as those hosted by health organizations, provide additional support. These platforms allow individuals to ask questions, share experiences, and receive advice from both peers and professionals.
Access to reliable online educational resources and support tools enhances patient knowledge and management of heart disease.
Frequently Asked Questions

Heart disease includes several types with different causes and treatments. Advances in medical science have improved treatments and recovery chances.
What are the different types of heart disease?
Heart disease comes in various forms. The most common types include coronary artery disease, arrhythmias, heart failure, and valvular heart disease. Each affects the heart in different ways. For example, coronary artery disease involves blocked or narrowed arteries, while arrhythmias are irregular heartbeats.
What are the primary causes of heart disease?
Heart disease can be caused by many factors. Common causes include smoking, high blood pressure, high cholesterol, diabetes, and obesity. Family history of heart disease can also increase the risk. Lifestyle choices such as lack of exercise and poor diet are significant contributors.
How can heart disease be treated?
Treatment for heart disease depends on the type and severity. Options include lifestyle changes, medications, and medical procedures. Lifestyle changes may involve diet and exercise improvements. Medications can manage symptoms and prevent complications. Medical procedures like angioplasty or heart surgery might be necessary for severe cases.
What are the latest advancements in the treatment of heart disease?
New treatments are continually being developed. Advances include minimally invasive surgeries, better medications, and improved diagnostic tools. For example, robotic-assisted surgeries and new heart stents have made procedures safer and more effective. Progress in genetics is also helping to predict and treat heart disease more precisely.
Is it possible to recover from heart disease?
Recovery from heart disease is possible with proper treatment and lifestyle changes. Many patients live healthy lives after treatment. Cardiac rehabilitation programs can help patients recover and improve their heart health. These programs include exercise training, education, and counseling.
How long can a person live with heart disease?
Lifespan with heart disease varies by individual. Factors include the type of heart disease, severity, and how well it is managed. With early diagnosis and proper treatment, many people live long, fulfilling lives. Regular medical check-ups and adhering to treatment plans are critical for longevity.