Prevention of genitourinary diseases involves a series of proactive measures that address lifestyle, awareness, and early detection to promote urinary tract and reproductive health. The genitourinary system—encompassing organs such as the kidneys, bladder, ureters, uterus, and reproductive organs—is complex. Maintaining its health is critical.
Healthy habits like regular hydration, proper hygiene, safe sexual practices, and avoiding tobacco use can significantly reduce the risk of developing genitourinary disorders.
Risk factors for genitourinary diseases can include a range of both controllable and uncontrollable elements. Individuals with a family history of such diseases, older age, or hormonal imbalances may be more susceptible. Nevertheless, recognizing early signs and symptoms, such as changes in urinary habits or unexplained pain, can lead to timely diagnosis and more effective treatment.
Regular health check-ups and screenings play an important role in early detection, especially for high-risk populations.
Key Takeaways
- Proactive lifestyle adjustments reduce the risk of genitourinary disorders.
- Awareness of personal risk factors aids in prevention and early detection.
- Recognizing symptoms promptly can lead to timely and effective treatment.
Understanding the Genitourinary System
Understanding the genitourinary system is essential for comprehending how the body maintains both reproductive and excretory functions. This section aims to elucidate the basic anatomy and function of this complex system, and its integral role in overall health.
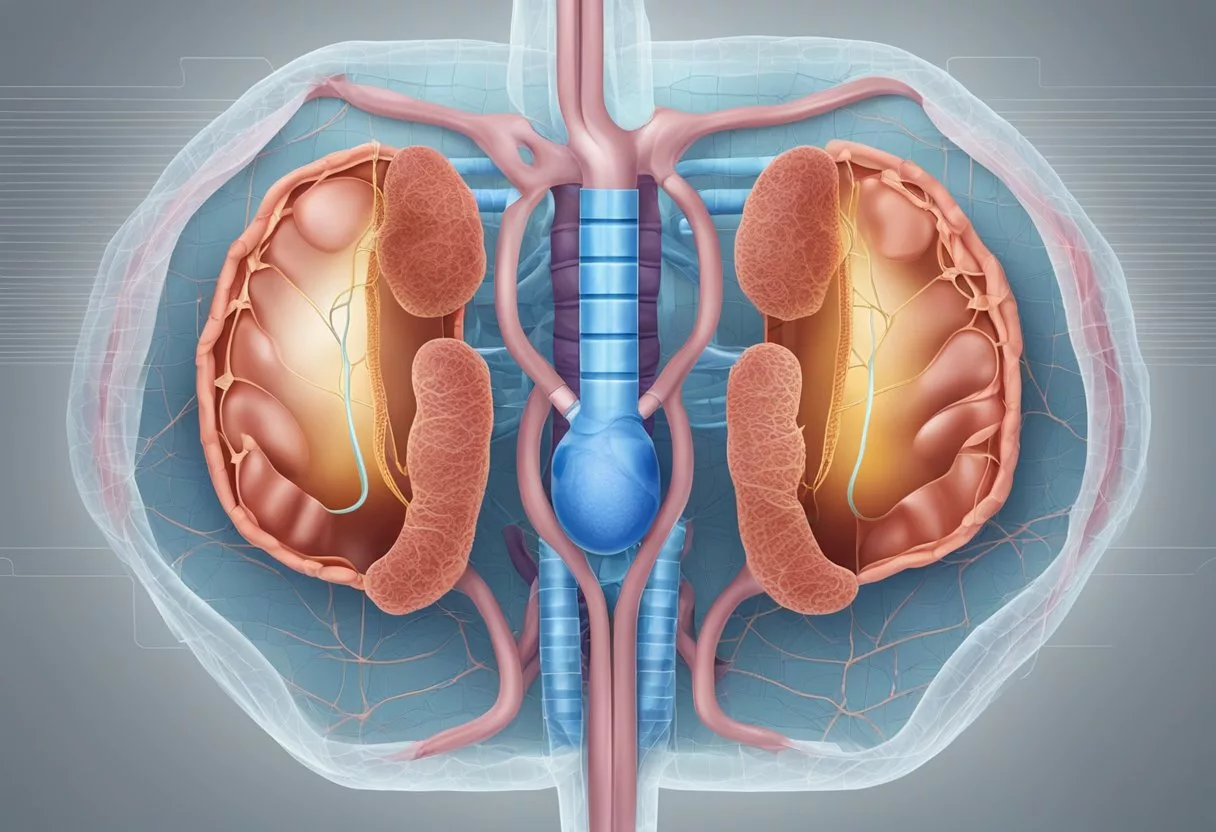
Basic Anatomy and Function
The genitourinary system is an intricate network that combines the urinary system—comprising the kidneys, ureters, bladder, and urethra—with the reproductive system, which includes organs such as the prostate, penis, and testicles in males, and the vagina, cervix, uterus, ovaries, and fallopian tubes in females.
- Kidneys: Vital for filtering waste from the bloodstream and regulating fluid balance.
- Ureters: Tubes that transport urine from the kidneys to the bladder.
- Bladder: A muscular sac that stores urine before elimination.
- Urethra: Conducts urine from the bladder out of the body.
In the male reproductive system, the penis and urethra are involved in both urination and ejaculation of semen, which is produced by the testicles, epididymis, and seminal vesicles. The female reproductive system includes the vagina, which serves as the birth canal and the passage for menstrual flow, while the cervix connects the vagina to the uterus, the site of fetal development. The ovaries produce eggs and reproductive hormones, and the fallopian tubes transport eggs from the ovaries to the uterus.
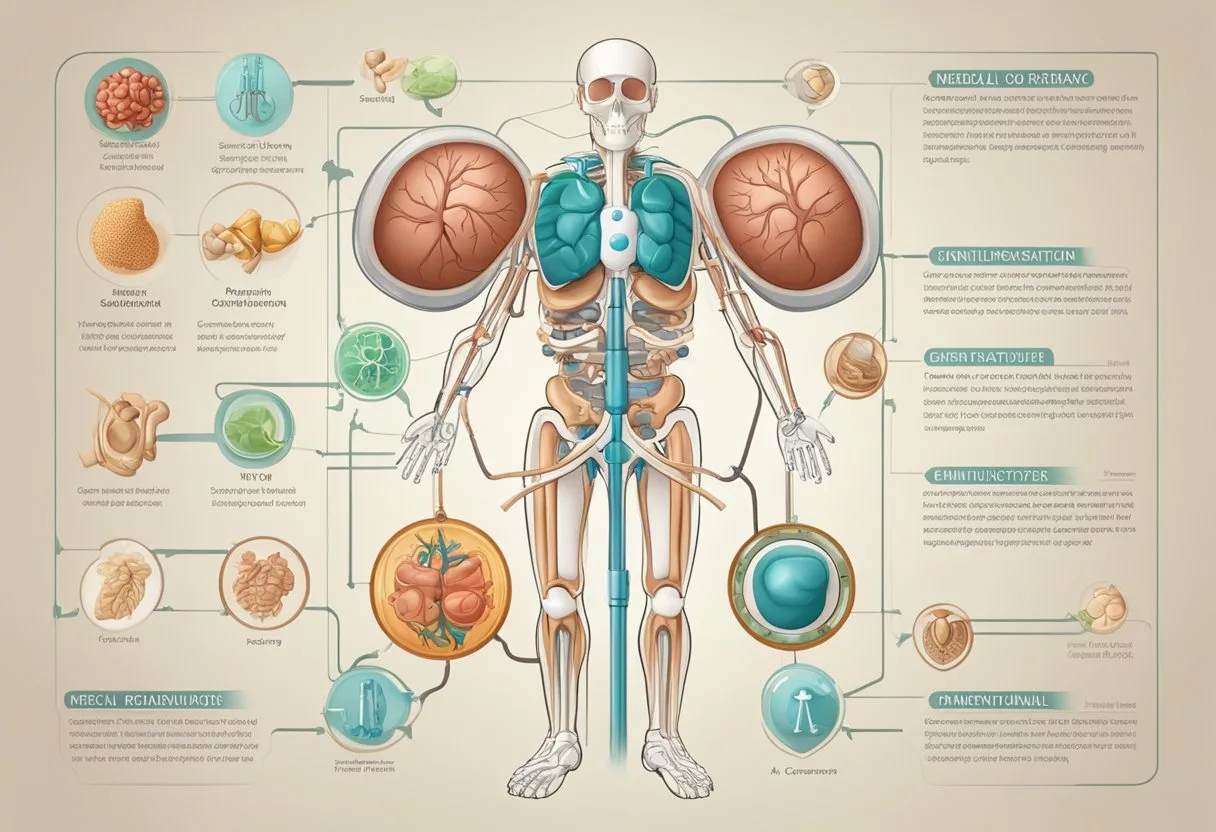
Role in Overall Health
The genitourinary system plays a critical role in maintaining homeostasis and facilitating reproductive functions. It eliminates waste products, manages electrolytes and blood pressure, and regulates hormones.
- Proper function is crucial for the overall health, affecting everything from waste excretion to sexual reproduction.
- Healthy kidneys filter and balance the blood composition, while the other components together ensure the propulsion and excretion of urine.
Common Genitourinary Disorders
Common genitourinary disorders encompass a range of conditions that can affect the urinary and reproductive organs. These disorders are often categorized by their nature—such as infections, structural issues, or cancers—and can significantly impact an individual’s quality of life.
Infections and Inflammations
Infections like urinary tract infections (UTIs) are prevalent genitourinary disorders, particularly in women, who have a shorter urethra. A UTI can occur in any part of the urinary system, with cystitis affecting the bladder and urethritis impacting the urethra. Vaginitis denotes inflammation of the vagina, often caused by a bacterial, viral, or yeast infection. Genitourinary syndrome of menopause is another condition that can lead to inflammatory changes in the female genitourinary tract, particularly due to estrogen deficiency.
Structural Abnormalities
Structural abnormalities in the genitourinary system can cause various symptoms and complications. Vesicoureteral reflux is a condition where urine flows backward from the bladder to the kidneys, leading to potential kidney damage. A neurogenic bladder occurs when neurological conditions disrupt nerve signals involved in bladder control, causing retention or incontinence. These abnormalities may be congenital or result from injury or illness.
Cancers and Tumors
The genitourinary system can be affected by different cancers and tumors, impacting organs such as the kidneys, bladder, and the reproductive organs. Early detection and treatment are critical for patient outcomes. For example, smoking is a known risk factor for bladder and kidney cancer. The presence of tumors within the genitourinary tract requires thorough medical evaluation to determine malignancy and appropriate treatment strategies.
Lifestyle and Prevention
Incorporating certain lifestyle choices can play a pivotal role in the prevention of genitourinary diseases. Focusing on exercise, weight management, and dietary choices, as well as avoiding smoking, can reduce risks associated with obesity, sexually transmitted diseases, and other related health concerns.
Healthy Habits
Diet: A balanced diet rich in fruits, vegetables, and whole grains contributes to overall health and supports the immune system. Limiting intake of processed foods and red meats, while including antioxidants and anti-inflammatory foods, can help prevent conditions such as urinary tract infections and kidney stones. It’s advisable to reduce consumption of caffeine and alcohol as these can irritate the bladder.
Smoking Cessation: It is well-established that smoking increases the risk of cancers in the genitourinary system, such as kidney, bladder, and cervical cancer. Those who quit smoking greatly reduce their risk for these diseases.
Sexual Health: Engaging in safe sexual intercourse, using condoms, and regular screening for sexually transmitted diseases are key measures in preventing infections that can lead to genitourinary complications.
Exercise and Weight Management
Exercise: Regular physical activity is essential in maintaining a healthy weight, which can prevent obesity—a significant risk factor for genitourinary diseases like prostate enlargement, kidney stones, and urinary incontinence. Exercise can also help reduce stress levels, another factor that can affect genitourinary health.
Weight Management: Maintaining a healthy weight through a combination of diet and regular exercise reduces the risk of developing obesity-related genitourinary disorders. Strategic weight management may prevent the onset of conditions like urinary incontinence, where excessive body weight places added pressure on the pelvic floor muscles.
Risk Factors and Early Detection
Effective prevention and management of genitourinary diseases hinge on recognizing the various risk factors associated with these conditions and the importance of early detection through regular screenings.
Identifying High-Risk Individuals
Risk factors that increase the likelihood of developing genitourinary diseases include diabetes, high blood pressure, and heart disease. Individuals who have these chronic conditions should be vigilant about their urogenital health. Smoking is another significant risk factor that can exacerbate the incidence of such diseases. Healthcare providers can assess individual risk by considering these conditions alongside a patient’s lifestyle habits and family history.
Screening and Regular Check-Ups
For early detection, routine screening is critical. High blood pressure should be monitored regularly as it can be an indicator of kidney issues. A physical exam, pelvic exam for women, and digital rectal exam for men can uncover abnormalities in the genitourinary system that may signify disease. For women, a Pap smear plays a crucial role in detecting early signs of cervical abnormalities, thereby facilitating timely intervention. It is recommended that those at risk or over a certain age attend regular check-ups, including these screenings, to ensure any potential issues are flagged and treated as early as possible.
Symptoms and Signs to Watch For
It is vital to recognize the manifestations of genitourinary disorders early, as they often indicate the body’s distress signals concerning urinary or reproductive system health.
Urinary Changes
Frequent or Urgent Urination: Individuals may experience an overwhelming need to urinate more often than usual or a sudden, strong urge to urinate, which could be a sign of a genitourinary disorder.
Urinary Incontinence: Leaking or dribbling of urine, either in small or large amounts, can occur unexpectedly in individuals with genitourinary issues.
Trouble Emptying the Bladder Completely: This feeling may persist even post-urination, suggesting that the bladder is not fully voiding.
Pain or Burning During Urination: Any discomfort, such as a burning sensation or pain, signifies that medical attention may be warranted.
Reproductive Concerns
Erectile Dysfunction: Men may encounter problems achieving or maintaining an erection, which can be a symptom of underlying genitourinary conditions.
Tenderness in the Lower Abdomen: One could feel pain or tenderness in the pelvic or lower abdominal area, indicative of potential infections or other genitourinary issues.
Individuals should consult a healthcare provider if they observe any of these symptoms to ensure timely and appropriate treatment.
Diagnosing Genitourinary Diseases

Early and accurate diagnosis of genitourinary diseases is crucial for effective treatment.
Physicians employ a variety of methods to diagnose these conditions.
Physical and Diagnostic Exams
A thorough medical history and physical examination are the first steps in diagnosing genitourinary diseases.
The medical history may reveal past issues or genetic predispositions that can be key indicators of certain conditions.
During the physical exam, a healthcare provider may look for physical signs of disease such as swelling, tenderness, or abnormalities.
In addition, a range of diagnostic tests may be utilized:
- Urinalysis: This is a common test where urine is checked for the presence of blood, protein, and other substances, providing valuable clues to the patient’s condition.
- Blood tests: These can reveal kidney function, hormone levels, and the presence of infections or other diseases.
- Cystoscopy and ureteroscopy: These procedures involve the insertion of a scope to examine the bladder and ureters, allowing for direct visualization of these areas.
Advanced Imaging Techniques
For more detailed information about the structures of the genitourinary system, advanced imaging techniques are often recommended:
- Ultrasound: Utilized for creating images of the kidneys, bladder, and other parts of the urinary tract to detect abnormalities.
- CT scan and MRI: These provide detailed cross-sectional images of the body and can help identify tumors, stones, or other issues within the genitourinary tract.
- X-ray: Often used in conjunction with an intravenous pyelogram (IVP), where a dye is injected to better visualize the urinary tract on X-rays.
Each of these diagnostic tools plays a critical role in the detection and management of genitourinary diseases, facilitating prompt and appropriate treatment.
Treatment Options

Effective management of genitourinary disorders often involves specific treatment strategies tailored to the type and severity of the condition.
Optimal patient care may require the use of medication, surgical interventions, or a combination of approaches.
Medication and Antibiotics
For bacterial infections of the genitourinary system, including urinary tract infections (UTIs), antibiotics are the cornerstone of treatment.
They are chosen based on the type of bacteria present and the patient’s medical history.
In the case of chronic conditions like interstitial cystitis or prostatitis, prescription medications can help manage symptoms.
Moreover, genitourinary syndrome of menopause (GSM) may benefit from estrogen therapy, which comes in various forms such as topical creams.
- UTIs: Specific antibiotics such as nitrofurantoin or ciprofloxacin are prescribed based on sensitivity tests.
- GSM: Vaginal estrogen creams or tablets can alleviate symptoms by replenishing local estrogen levels.
Surgical Interventions
Certain genitourinary disorders may require surgical treatments to restore function or remove abnormalities.
For example, cancer of the genitourinary tract, such as prostate or bladder cancer, might be treated with surgery to remove the tumor.
This is often followed by additional cancer treatments like chemotherapy or radiation therapy.
- Cancer: Surgical resection of the tumor is often the first line of action, which may be combined with chemotherapy or radiation.
- Obstructions: Conditions causing a blockage, like kidney stones, may necessitate surgical intervention to remove the obstruction.
Complications and Management

Proper management of genitourinary diseases is crucial to prevent complications such as chronic kidney disease, urinary obstructions, and infertility.
Effective handling of these conditions requires prompt attention to acute episodes and steady monitoring of chronic conditions to preserve urinary tract health and kidney function.
Dealing with Chronic Conditions
Chronic conditions within the genitourinary system, such as chronic kidney disease or long-term inflammation, necessitate ongoing management to maintain kidney function and prevent progression.
Strategies include:
- Regular Monitoring: Scheduled check-ups to assess kidney function and detect changes early.
- Diet and Lifestyle: Adjustments to diet and lifestyle to decrease the workload on the kidneys and reduce risks of further complications.
Handling Acute Episodes
Acute episodes, like urinary obstructions or sepsis, are serious and require immediate medical intervention.
Key management steps include:
- Prompt Diagnosis: Rapid identification using imaging and laboratory tests to ascertain the cause.
- Immediate Treatment: Addressing the root of the issue, which might involve antibiotics for infections or surgery for obstructions, is essential to prevent lasting damage to the urinary tract and preserve fertility.
Pediatric and Adolescent Considerations

In pediatric and adolescent populations, the prevention of genitourinary diseases requires a tailored approach.
Children’s anatomical and physiological differences, along with the unique risks during these developmental stages, necessitate specific strategies and careful monitoring.
Special Concerns for the Younger Population
The young population, particularly children, have anatomical and physiological differences that can predispose them to certain genitourinary conditions.
For instance, vesicoureteral reflux is a condition more common in children, characterized by the abnormal flow of urine from the bladder back into the ureters, and potentially to the kidneys.
This backflow can lead to frequent urinary tract infections (UTIs), which, if left untreated, may cause kidney damage. Regular monitoring and early detection are crucial to managing this condition.
Furthermore, during pregnancy, women experience significant changes that can increase the risk of UTIs.
The expanding uterus can put pressure on the bladder, making complete emptying more difficult and promoting infection.
Pregnant women should have regular urine screenings to detect asymptomatic bacteriuria, which can lead to more serious infections if not addressed.
Recognizing symptoms early in children, such as fever or irritability, may indicate a genitourinary infection, even when traditional symptoms like dysuria are absent.
Pediatric care providers should maintain a high index of suspicion when such non-specific symptoms are present.
Information on the importance of recognizing early symptoms is outlined in an article from The Clinics of North America.
Pediatric patients facing genitourinary issues also benefit from the knowledge that their anatomy and function will change as they grow and develop.
Healthcare providers should guide families on the expected changes and how to adapt prevention strategies accordingly.
For adolescents, proper education about personal hygiene, the risks of sexually transmitted infections, and the importance of safe practices can prevent a multitude of genitourinary disorders.
Adolescents should also be encouraged to seek medical advice when experiencing unusual symptoms in order to treat potential infections or other conditions before they progress.
Women’s Genitourinary Health

Women’s genitourinary health encompasses a broad array of conditions that uniquely affect the female urinary tract and reproductive system.
Careful attention to these areas can help alleviate and prevent common and unique health challenges faced by women.
Unique Female Conditions
The female genitourinary tract has distinctive conditions, often influenced by anatomical structure, hormonal fluctuations, and life stages.
For example, the vagina is an elastic, muscular canal with a soft, flexible lining that provides lubrication and sensation.
Conditions like bacterial vaginosis and yeast infections are more prevalent due to the vagina’s specific pH and microbiome.
Women are also more susceptible to urinary tract infections (UTIs) due to a shorter urethra, which can make maintaining genitourinary hygiene especially important.
During pregnancy, the risk of UTIs increases because of hormonal changes and the physical pressure of the growing uterus on the bladder.
| Condition | Description | Relevance |
|---|---|---|
| Bacterial Vaginosis | An imbalance of vaginal bacteria | Common in women of childbearing age |
| UTIs | Infection in urinary tract | Shorter urethra increases risk |
| Yeast Infections | Fungal overgrowth in vagina | Affected by hormonal changes, antibiotics, and personal hygiene |
Reproductive Health and Menopause
Reproductive health is pivotal in a woman’s life, with menopause being one of the most significant transitions.
During menopause, women can experience genitourinary syndrome of menopause (GSM), which entails symptoms such as vaginal dryness, itching, and irritation.
GSM is a direct result of the decrease in estrogen levels, affecting the elasticity and lubrication of the vaginal tissue.
Women’s health strategies during menopause often focus on mitigating these symptoms, sometimes employing hormone replacement therapy or non-hormonal moisturizers and lubricants.
| Menopause Symptom | Description | Management Strategy |
|---|---|---|
| Vaginal Dryness | Decreased lubrication leading to discomfort | Use of vaginal moisturizers or lubricants |
| Vaginal Atrophy | Thinning of vaginal walls | Estrogen therapy or non-hormonal options |
| Urinary Symptoms | Frequency, urgency, incontinence | Pelvic floor exercises, bladder training, medication |
Men’s Genitourinary Health

Men’s genitourinary health encompasses a range of conditions that affect the male reproductive organs and the urinary tract. It’s important for individuals to understand the unique aspects of male genitourinary health.
These include how to maintain it and how it can change with aging.
Unique Male Conditions
Male-specific genitourinary conditions largely revolve around the prostate and testicles. The prostate is prone to several conditions that can impact urinary function and sexual health.
For example, Benign Prostatic Hyperplasia (BPH), or an enlarged prostate, can lead to symptoms such as frequent urination, difficulty starting urination, or weak urine flow. Regular screening is vital as men age since the risk of prostate cancer also increases over time.
The testicles are responsible for the production of sperm and testosterone.
Conditions like testicular cancer, although less common, require awareness and timely action. Testicular self-exams can help men detect abnormalities early.
Reproductive Health and Aging
As men age, changes in reproductive health are inevitable. The quantity and quality of sperm production can decline, potentially affecting fertility.
Erectile function commonly changes with age; erection difficulties can become more frequent. It’s important for aging men to discuss these changes with healthcare providers as they may be indicative of underlying health issues such as cardiovascular disease or diabetes.
Both preventive care and treatment options exist to help men maintain their genitourinary health as they age.
Lifestyle changes, medical screenings, and medications may play a role in managing symptoms and conditions.
Frequently Asked Questions

When it comes to genitourinary diseases, prevention is always preferable to treatment. This section addresses commonly asked questions on how to proactively reduce the risk of such conditions through lifestyle changes, dietary considerations, and personal hygiene practices.
What are effective prevention methods for common urinary tract infections?
Preventing urinary tract infections (UTIs) often involves a combination of hydration and urination habits.
Individuals are advised to drink plenty of water and urinate frequently to flush bacteria from the urinary system. Cranberry juice or supplements may also reduce the risk of UTIs by preventing bacteria from adhering to the urinary tract walls.
What lifestyle changes can reduce the risk of developing kidney stones?
Reducing the risk of kidney stones typically requires staying well-hydrated, limiting salt intake, and reducing consumption of high-oxalate foods like spinach and almonds.
Incorporating calcium-rich foods in a balanced way can also help minimize the formation of certain types of kidney stones.
How can routine screening help in preventing genitourinary cancers?
Routine screening can aid in the early detection and prevention of genitourinary cancers, such as prostate, kidney, and bladder cancer.
Methods like PSA tests for prostate cancer increase the likelihood of successful treatment and can prevent the progression of the disease.
What dietary modifications can aid in the prevention of genitourinary diseases?
Diet plays a crucial role in the health of the genitourinary system. A diet high in fruits, vegetables, and whole grains, while low in red and processed meats, is associated with decreased risk of issues like cancer and chronic kidney disease.
Which hygiene practices are recommended to minimize the risk of genitourinary infections?
Maintaining proper hygiene is key to preventing genitourinary infections.
Regular bathing, wearing breathable cotton underwear, and for women, wiping from front to back, can decrease the likelihood of bacterial spread and infection.
What are the benefits of pelvic floor exercises in preventing urinary incontinence?
Pelvic floor exercises, or Kegel exercises, strengthen the muscles that support the bladder. This improves bladder control and reduces the risk of urinary incontinence. Consistency with these exercises is vital for achieving and maintaining benefits.