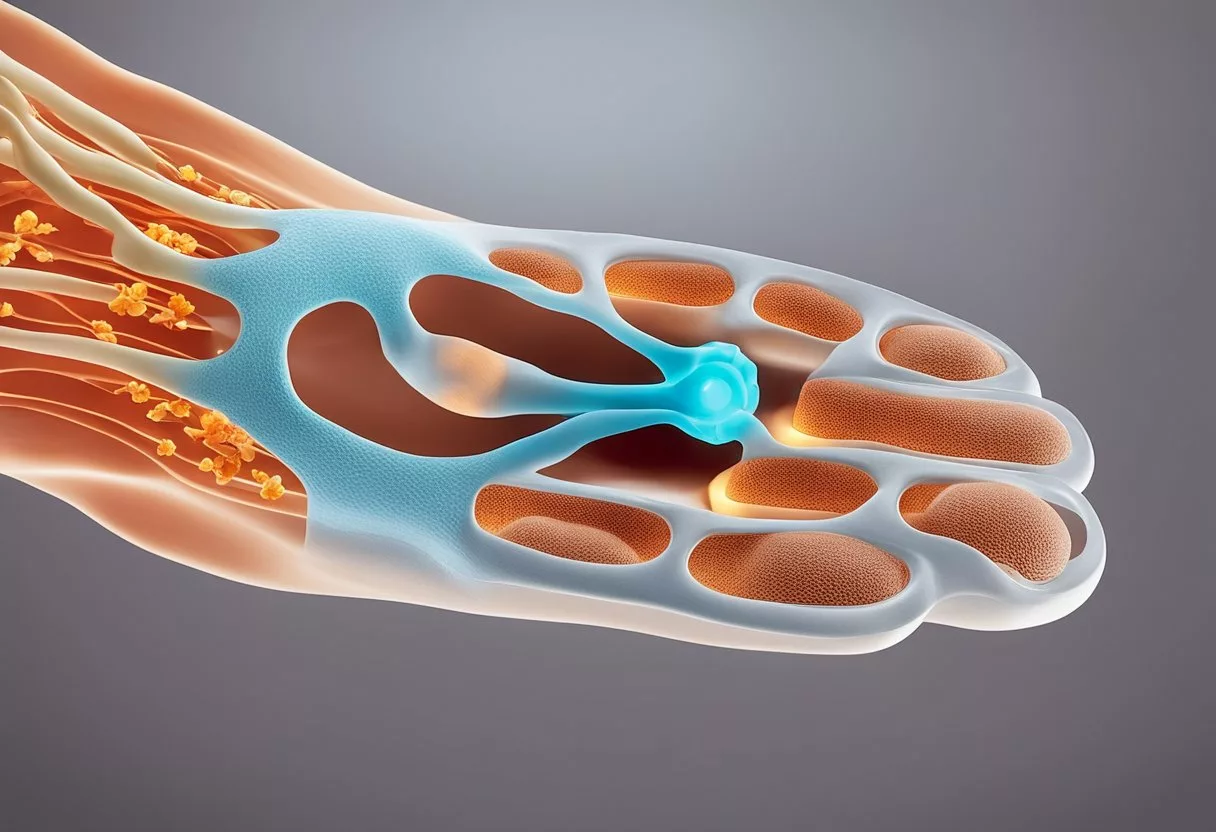
Plantar fasciitis is a prevalent cause of heel pain that affects a broad range of individuals. This condition stems from the inflammation of the plantar fascia, which is a dense band of tissue that runs along the bottom of the foot, connecting the heel bone to the toes.
When the plantar fascia is overstressed or overloaded, it can develop micro-tears, leading to pain and stiffness in the heel area. The discomfort is often most intense with the first steps after waking up, though it can also trigger after standing for long periods or when rising from sitting.
The diagnosis of plantar fasciitis largely relies on the patient’s history and physical examination. Symptoms typically present as a sharp or dull ache at the bottom of the heel, which can be aggravated by prolonged activity or exertion. Knowing the causes is essential in both treatment and prevention. Factors that contribute to the development of this condition include poor footwear, excessive weight, certain exercises, and anatomical issues. Treatment options vary, ranging from home remedies such as rest and ice to medical interventions like physical therapy, orthotics, and, in more severe cases, surgery. Recovery requires patience, as the condition can take several months to resolve, and understanding potential complications is vital to managing expectations.
Key Takeaways
- Plantar fasciitis is a common source of heel pain due to inflammation of the tissue running along the foot’s bottom.
- Diagnosis is based on symptoms and physical exam, and treatment ranges from self-care to professional medical interventions.
- Understanding the causes and implementing preventative measures is essential for managing plantar fasciitis effectively.
Understanding Plantar Fasciitis
In exploring plantar fasciitis, it’s crucial to look at its anatomical foundations and the factors that contribute to its development. This painful condition affects a vital part of the foot’s structure and is influenced by both physiological and lifestyle factors.
Definition and Anatomy
Plantar fasciitis is characterized by pain at the bottom of the heel or along the arch of the foot, primarily due to inflammation of the plantar fascia. The plantar fascia is a thick band of tissue that runs from the heel bone to the front of the foot, supporting the arch and absorbing the stresses we place on our feet.
- Tenderness in the heel or arch when touched
- Pain that is usually worse upon taking the first steps in the morning
- Decreasing pain after the first few steps, but potentially returning after long periods of standing or rising from being seated
Prevalence and Risk Factors
Plantar fasciitis commonly affects individuals between the ages of 40 and 60. However, it can occur in a wide range of populations with various risk factors:
- Age: Increased risk as the tissue becomes less elastic with age
- Weight: Higher incidence in those who are obese due to additional pressure on the plantar fascia
- Exercise: Activities like running that place a lot of stress on the heel and attached tissue can contribute to the onset
- Foot Mechanics: Both flat feet and high arches may predispose individuals to plantar fasciitis
- Occupation: Jobs that require long periods of standing or walking on hard surfaces can increase the risk
Individuals with certain biomechanical issues such as an uneven distribution of weight during walking or standing may also have an increased risk of developing plantar fasciitis. The proper management of these factors is crucial for both prevention and treatment.
Symptoms and Diagnosis
Understanding the symptoms of plantar fasciitis and the process involved in its diagnosis is crucial for individuals experiencing heel pain.
Identifying Symptoms
Individuals with plantar fasciitis typically report a sharp heel pain that is most noticeable with the first steps after waking in the morning or after extended periods of rest. This pain can decrease as they move more, but might return after long periods of standing or when standing up after sitting. The pain is often described as originating from the bottom of the heel and may be due to inflammation of the plantar fascia. Other common symptoms include:
- Stiffness in the foot, particularly in the morning
- Swelling on the bottom of the heel
- Tenderness when touching the heel or arch of the foot
Medical Diagnosis
To diagnose plantar fasciitis, a doctor will perform a physical exam to check for areas of tenderness in the foot, as this can help pinpoint the exact cause of the heel pain. They may observe how the pain changes with movement and position changes. While imaging tests are not typically necessary, they can be used to rule out other conditions. If required, an X-ray or ultrasound may be conducted to ensure there are no fractures or other abnormalities contributing to the pain.
Causes of Plantar Fasciitis
Plantar fasciitis is often the result of strain and inflammation in the foot’s plantar fascia. This strain can lead to tears in the tissue and may cause heel pain.
Biomechanical Factors
Biomechanical issues such as flat feet, high arches, or abnormal walking patterns can exert excessive tension on the plantar fascia. Over time, the stress from poor arch support may lead to microtears and inflammation in the tissue, contributing to the development of plantar fasciitis.
- Flat feet: May cause an uneven distribution of body weight, which puts added pressure on the plantar fascia.
- High arches: Can be less effective at absorbing shock, leading to increased stress on the plantar fascia.
- Abnormal walk patterns: Can disturb the weight distribution, causing additional strain on the foot.
Lifestyle and Health Conditions
Lifestyle choices and certain health conditions can also contribute to the risk of developing plantar fasciitis. Regular overuse of the foot due to intensive exercise or prolonged periods of standing can lead to inflammation and pain. Additional body weight, including from pregnancy or being overweight, can also increase the pressure on the plantar fascia.
- Exercise: High-impact activities such as running or jumping can lead to repeated strain.
- Weight: Extra pressure from body weight strains the plantar fascia, especially in overweight individuals.
- Pregnancy: Weight gain and hormonal changes during pregnancy can impact foot structure.
In some cases, systemic inflammatory conditions such as arthritis may also predispose individuals to plantar fasciitis due to the associated inflammation of the supporting foot structures.
Treatment Options

Effective management of plantar fasciitis involves a multifaceted approach, tailored to alleviate pain, reduce inflammation, and facilitate healing of the plantar fascia.
Conservative Treatments
For most individuals with plantar fasciitis, nonsurgical treatment methods are the cornerstone of recovery. Rest and ice application are initial steps to reduce inflammation and pain. Regular exercises and stretching of the Achilles tendon and plantar fascia can improve flexibility and strengthen the lower leg muscles, mitigating stress on the heel.
Use of night splints may help in keeping the plantar fascia gently stretched during sleep. Custom or over-the-counter orthotics provide the necessary support to distribute pressure more evenly across the foot. If heel spurs are present, they require specific adjustments in orthotics.
Physical therapy plays a significant role; specialists design an exercise regimen that ensures gradual stretching and strengthening of the plantar fascia, Achilles tendon, and intrinsic foot muscles.
Medications and Injections
Medical management often includes nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen to alleviate pain and inflammation. For more persistent cases, steroid injections, particularly corticosteroids, can provide temporary relief by reducing inflammation.
Surgical and Advanced Therapies
When conservative treatments are not effective and the pain persists for 6-12 months, surgical and advanced therapies might be considered. Surgery to release part of the plantar fascia may be recommended for persistent cases. Shock wave therapy is a non-invasive procedure that can stimulate healing within the fascia.
Gastrocnemius recession, a surgery to lengthen the calf muscles, is another option for patients who have difficulty with isolated stretching. These advanced treatments carry higher risks and are typically considered when all other treatments have not led to significant improvement.
Prevention and Management

Preventing plantar fasciitis involves a combination of lifestyle adjustments and targeted exercises that can strengthen foot musculature and enhance flexibility. These methods aim to minimize strain on the plantar fascia, reducing the risk of developing pain associated with plantar fasciitis.
Lifestyle Modifications
Rest is crucial for individuals experiencing early signs of heel pain, as ongoing stress on the feet can exacerbate plantar fasciitis. One should consider reducing activities like running, especially on hard surfaces, until symptoms improve. Instead, opting for low-impact exercises such as swimming or cycling can maintain fitness without placing undue pressure on the plantar fascia.
Wearing supportive shoes that provide proper arch support can significantly reduce the stress on the plantar fascia. Individuals should avoid walking barefoot on hard surfaces and choose footwear that cushions the heel and supports the arch of the foot. It may be beneficial to use orthotic inserts designed to distribute weight evenly and alleviate pain.
Maintaining an ideal weight is important as excessive body weight can increase strain on the plantar fascia. Overweight individuals should consider a weight management plan to lessen the impact on their feet during daily activities.
Exercise and Strengthening
Engaging in stretching exercises targets the calf muscles and the plantar fascia itself, enhancing flexibility and reducing tension. One can perform daily stretches such as:
- The calf stretch: Leaning forward against a wall, straighten one leg and bend the other, pushing the heel down towards the floor.
- The plantar fascia stretch: Seated with one leg crossed over the other, pull the toes towards the shin until a stretch is felt in the arch of the foot.
Strengthening the muscles in the feet can also prevent plantar fasciitis. Exercises like toe curls and doming involve curling the toes and arching the foot, and this can be done using a towel on the floor to add resistance. Regularly incorporating these exercises into one’s routine can help maintain foot health.
By combining prudent lifestyle modifications with a targeted exercise regimen, individuals can manage and possibly prevent the occurrence of plantar fasciitis, leading to sustained foot health and mobility.
Understanding Recovery and Complications
Recovery from plantar fasciitis is generally favorable with proper treatment, but patients should be aware of the typical healing timeline and potential complications that can arise during the recovery process.
Recovery Process
The recovery process for plantar fasciitis involves a period of rest and rehabilitation exercises aimed at reducing inflammation and pain. Typically, one can expect a progressive decrease in discomfort over several weeks to months. Key components of the recovery phase include:
- Consistent application of ice to reduce inflammation.
- The implementation of stretching exercises for the calf muscles and plantar fascia.
- The possible use of orthotic inserts or supportive footwear to alleviate pressure on the plantar fascia.
- In some cases, physical therapy may be recommended to guide recovery.
It’s crucial for patients to adhere to the prescribed treatment regimen to facilitate healing and prevent re-injury. The recovery time can vary, with some individuals experiencing symptom resolution within a few weeks, while others may take several months to fully recover.
Potential Complications
While most cases of plantar fasciitis resolve with conservative treatment, some individuals may experience complications which can extend recovery time and impact daily activities. Potential complications include:
- Chronic plantar fascia pain due to incomplete healing or ongoing strain.
- The development of stress fractures of the heel bone (calcaneus) from continuous stress without adequate rest.
- Persistent inflammation that may lead to ligament damage or changes in foot structure.
- Rarely, chronic plantar fasciitis can lead to nerve damage if the condition is not addressed properly.
Patients are encouraged to follow their healthcare provider’s advice closely and report any persistent or worsening symptoms to avoid long-term complications.
When to See a Doctor
In the journey of managing plantar fasciitis, an individual must consider seeking medical advice when certain symptoms persist or worsen. They should consult a doctor if they experience severe pain or swelling that limits daily activities and does not improve with rest, ice, and over-the-counter treatments.
- Persistent Discomfort: If discomfort in the heel or the bottom of the foot persists for more than a week, despite attempts at home care.
- Pain that Worsens: A sensation that the pain is intensifying over time or is particularly severe when taking the first steps after waking up, or after prolonged periods of sitting or standing.
- Stiffness and Limited Range of Motion: Difficulty in flexing the foot, pointing toes towards the shin (dorsiflexion), which may involve the Achilles tendon.
A healthcare provider can diagnose plantar fasciitis through a physical examination and evaluate the need for imaging tests. Diagnosis is typically made by assessing tenderness and swelling in specific areas of the foot. A doctor may also check for the proper functioning of the foot and the Achilles tendon to determine the cause of the discomfort and pain.
Visiting a doctor is crucial for receiving a proper diagnosis and exploring a variety of treatment options tailored to the patient’s condition. The healthcare professional may recommend specific exercises, orthotics, medications, or in some cases, more advanced treatments like physical therapy or surgery. It is best to address the symptoms of plantar fasciitis early to prevent chronic heel pain and to facilitate a faster recovery.
Innovations in Treatment
Plantar fasciitis treatment has advanced with the introduction of shock wave therapy (SWT). This non-invasive method utilizes sound waves to stimulate healing within the plantar fascia. Studies suggest SWT can be particularly effective for chronic cases that do not respond to more conservative treatments.
Physical therapy has also seen innovation through tailored exercise regimens. These are crafted focusing on:
- Stretching: Specifically designed exercises that target the Achilles tendon and plantar fascia to alleviate tension.
- Strengthening: Exercises aimed at reinforcing the muscles that support arch stability.
Injections have evolved beyond corticosteroids, with options like platelet-rich plasma (PRP) emerging. This treatment involves injecting a concentration of the patient’s own platelets to promote healing of injured tendons, ligaments, muscles, and joints, potentially offering a more naturally derived avenue for tissue repair.
Physical therapists now often incorporate advanced technologies and techniques in their practice, such as:
- Ultrasound-guided techniques: To improve accuracy of injections.
- Graston Technique: Utilizing specialized tools to assist in breaking down fascial restrictions and scar tissue.
While these treatments can be effective, it is essential to assess their appropriateness on an individual basis. Healthcare providers typically recommend a comprehensive approach that combines these new treatments with proven methods for optimal results.
Patient Testimonials and Case Studies
Patient testimonials and case studies on plantar fasciitis showcase real-world experiences, highlighting both the triumphs in healing and recovery, as well as the potential complications and discomforts that can arise during treatment.
Success Stories
Individuals who have recovered from plantar fasciitis often emphasize the effectiveness of comprehensive, consistent treatment regimens. In one case, a middle-aged runner utilized a combination of rest, physical therapy, and custom orthotics to alleviate her symptoms. After six months of diligent application, she reported a complete cessation of heel pain and stiffness, signifying a full recovery.
Key factors in successful case studies include:
- Adherence to prescribed treatment plans
- Incorporation of stretching and strengthening exercises
- Use of supportive footwear or orthotic inserts
- Patience with the recovery timeline, typically spanning several months
Challenges in Treatment
Conversely, patients can face difficulties during their treatment journey. It is not uncommon for some individuals to experience prolonged discomfort or complications that hinder recovery. A patient case highlighted the challenges of treating plantar fasciitis when underlying health issues, such as obesity, exacerbate the condition. This patient’s recovery was impeded by persistent tendon stiffness and additional strain on his feet due to excess weight, requiring an extended treatment duration and more aggressive interventions, such as corticosteroid injections.
Reported challenges include:
- Delay in symptom improvement, leading to frustration and decreased motivation
- Complications from comorbid conditions, such as diabetes or arthritis
- Requirement for more invasive treatments if initial conservative measures are unsuccessful
Frequently Asked Questions
This section addresses common inquiries regarding the symptoms, home treatments, and pain management strategies for plantar fasciitis, as well as guidance on activities and recovery indicators.
What are the typical symptoms of plantar fasciitis?
The hallmark symptom of plantar fasciitis is a sharp, stabbing heel pain, particularly noticeable with the first steps after awakening or after prolonged periods of inactivity. It may also manifest as a throbbing pain after extended periods of standing.
How can plantar fasciitis be treated effectively at home?
Home treatment for plantar fasciitis includes rest, ice application to reduce inflammation, use of over-the-counter pain relievers, and maintaining a healthy weight. Supportive shoes and the use of orthotic inserts can also provide relief.
Which stretches are recommended for relieving plantar fasciitis pain?
Stretching exercises for plantar fasciitis focus on the Achilles tendon and plantar fascia. One common stretch involves leaning forward against a wall with one knee straight and heel on the ground, then bending the other knee. This stretches the fascia and should be done several times a day, especially before taking the first steps in the morning.
Are there specific activities to avoid when suffering from plantar fasciitis?
Individuals with plantar fasciitis should avoid high-impact activities such as running and jumping that may exacerbate heel pain. They should also avoid walking barefoot on hard surfaces, which can increase the strain on the plantar fascia.
What are the best pain relief options for managing plantar fasciitis?
The most effective pain relief methods include nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen. Localized treatments such as ice massages, corticosteroid injections, and sometimes ultrasound therapy are used to alleviate pain and reduce inflammation.
How can one identify that their plantar fasciitis is healing?
Healing is typically indicated by a gradual decrease in heel pain, especially in the morning or after sitting for extended periods. Increased ease in performing daily activities without discomfort also suggests improvement in the condition.